Abstract
Background
Acquiring operative skills in the course of a structured neurosurgery residency training program is vital to safely operating on patients autonomously upon board certification. We tested the hypothesis that the complication rates and outcome of microscopic lumbar spinal stenosis (LSS) decompression done by supervised residents are not inferior to those of board-certified faculty neurosurgeons (BCFNs).
Methods
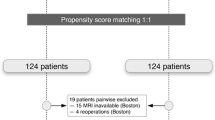
Retrospective single-center study performed at a Swiss teaching hospital comparing consecutive patients undergoing surgery for LSS by a supervised neurosurgery resident (teaching cases) to a consecutive series of patients operated on by a BCFN (non-teaching cases). The primary endpoint was occurrence of complications during surgery. Secondary endpoints were patients’ clinical outcomes 4 weeks after surgery, categorized into a binary responder and non-responder variable, occurrence of postoperative complications, need for re-do surgery, and clinical outcome until the last follow-up (FU).
Results
In a total of n = 471 operations, n = 194 (41.2 %) were teaching cases and n = 277 (58.8 %) non-teaching cases. A longer operation time (single-level procedures: mean 100.0 vs. 83.2 min, p < 0.001) was recorded for teaching cases, while estimated blood loss was equal (single-level procedures: mean 109.9 vs. 117.0 ml, p = 0.409). In multivariate analysis, supervised residents were as likely as BCFNs to have an intraoperative complication (OR 0.92, 95 % CI 0.41–2.04, p = 0.835). They were as likely as BCFNs to achieve a favorable 4-week response to surgery (OR 1.82, 95 % CI 0.79–4.15, p = 0.155). Until final FU, the likelihood for patients in the teaching group to suffer from postoperative complications (OR 1.07, 95 % CI 0.46–2.49, p = 0.864) or require re-do surgery (OR 0.68, 95 % CI 0.31–1.52, p = 0.358) was similar to that of the non-teaching group.
Conclusions
Complication rates and short- and mid-term outcomes following LSS decompression were comparable for patients operated on by supervised neurosurgery residents and senior neurosurgeons. Our data thus indicate that a structured neurosurgical hands-on training including LSS decompression is safe for patients.

Similar content being viewed by others
References
Schaller K (2013) Neurosurgical training under European law. Acta Neurochir (Wien) 155:547
Stienen MN, Netuka D, Demetriades A, Ringel F, Gempt J, Gautschi OP, Kuhlen DE, Schaller K (2015) Neurosurgical resident education in Europe—results of a multinational survey. Acta Neurochir (Wien). doi:10.1007/s00701-015-2632-0
Stienen MN, Netuka D, Demetriades A, Ringel F, Gempt J, Gautschi OP, Kuhlen DE, Schaller K (2015) Working Time of Neurosurgical Residents in Europe—results of a multinational survey. Acta Neurochir (Wien) accepted for publication (Wien). doi:10.1007/s00701-015-2633-z
Lindsay K (2012) Accreditation of neurosurgical training programmes in Europe: report of JRAAC. Acta Neurochir (Wien) 154:947–949
Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Gautschi OP (2014) Early surgical education of residents is safe for microscopic lumbar disc surgery. Acta Neurochir (Wien) 156:1205–1214
Stienen MN, Smoll NR, Tessitore E, Schaller K, Hildebrandt G, Gautschi OP (2015) Surgical resident education in non-instrumented lumbar spine surgery: a prospective observational study with a 4.5-year follow-up. World Neurosurg. doi:10.1016/j.wneu.2015.07.030
Stienen MN, Joswig H, Jucker D, Hildebrandt G, Schaller K, Gautschi OP (2015) Anterior cervical discectomy and fusion: is surgical education safe? Acta Neurochir (Wien). doi:10.1007/s00701-015-2396-6
Wiese M, Kramer J, Bernsmann K, Ernst Willburger R (2004) The related outcome and complication rate in primary lumbar microscopic disc surgery depending on the surgeon's experience: comparative studies. Spine J 4:550–556
Gautschi OP, Stienen MN, Smoll NR, Corniola MV, Tessitore E, Schaller K (2014) Incidental durotomy in lumbar spine surgery—a three-nation survey to evaluate its management. Acta Neurochir (Wien) 156:1813–1820
Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS (1998) Interpreting treatment effects in randomised trials. BMJ 316:690–693
Bydon M, Abt NB, De la Garza-Ramos R, Macki M, Witham TF, Gokaslan ZL, Bydon A, Huang J (2015) Impact of resident participation on morbidity and mortality in neurosurgical procedures: an analysis of 16,098 patients. J Neurosurg 122:955–961
Knifed E, Taylor B, Bernstein M (2008) What surgeons tell their patients about the intraoperative role of residents: a qualitative study. Am J Surg 196:788–794
McAlister C (2015) Breaking the silence of the switch—increasing transparency about trainee participation in surgery. N Engl J Med 372:2477–2479
Nerland US, Jakola AS, Solheim O, Weber C, Rao V, Lonne G, Solberg TK, Salvesen O, Carlsen SM, Nygaard OP, Gulati S (2015) Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ 350:h1603
Giannadakis C, Hammersboen LE, Feyling C, Solheim O, Jakola AS, Nerland US, Nygaard OP, Solberg TK, Gulati S (2015) Microsurgical decompression for central lumbar spinal stenosis: a single-center observational study. Acta Neurochir (Wien) 157:1165–1171
Mannion AF, Fekete TF, O'Riordan D, Porchet F, Mutter UM, Jeszenszky D, Lattig F, Grob D, Kleinstueck FS (2013) The assessment of complications after spine surgery: time for a paradigm shift? Spine J 13:615–624
Acknowledgments
The authors thank all the trusting patients who agreed to be operated on by a supervised resident and contributed to their training. We likewise thank all the BCFNs for teaching the art of surgery.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Funding
No funding was received for this research.
Ethics approval
No formal consent is required for this type of study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Holger Joswig and Carolin Hock contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 39 kb)
Rights and permissions
About this article
Cite this article
Joswig, H., Hock, C., Hildebrandt, G. et al. Microscopic lumbar spinal stenosis decompression: is surgical education safe?. Acta Neurochir 158, 357–366 (2016). https://doi.org/10.1007/s00701-015-2667-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2667-2