Abstract
Background
Tandem intracranial aneurysms are aneurysms located along a single intracranial vessel. Adjacent tandem aneurysms arise within the same vascular segment and their presence often suggests diffuse parent vessel anomaly. Endovascular management of these rare lesions has not been well studied. In this retrospective observational study, we describe our experience treating adjacent tandem intracranial aneurysms with endovascular embolization.
Methods
We retrospectively reviewed records of patients with these lesions who underwent endovascular treatment between 2008 and 2013.
Results
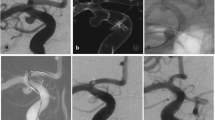
Thirteen patients (mean age 60.8 years; 12 women) with 28 adjacent tandem aneurysms were treated during the study timeframe. Aneurysms were located along the clinoidal, ophthalmic, and communicating segments of the internal carotid artery in 12 patients and at the basilar apex in one patient. Average size was 8.4 mm. Six patients (12 aneurysms) were treated by flow diversion via the Pipeline embolization device (PED) and seven (16 aneurysms) by stent-assisted coiling, with coils successfully placed in 11 aneurysms. Clinical follow-up was available for an average of 26.1 months; postprocedural angiography was performed for 12 patients. Complete occlusion was achieved in nine of ten (90 %) PED-treated aneurysms and eight of 11 (72.7 %) treated by stent-assisted coiling (p = 0.44). Two patients treated by stent-assisted coiling required re-coiling for aneurysm recanalization. Overall, modified Rankin scale scores were 0–1 for 12 patients and 3 for one patient.
Conclusions
Adjacent tandem intracranial aneurysms can be safely and effectively treated by either stent-assisted coiling or flow diversion. We prefer PED flow diversion due to better parent vessel reconstruction and lower recanalization risk.



Similar content being viewed by others
References
Baccin CE, Krings T, Alvarez H, Ozanne A, Lasjaunias P (2006) Multiple mirror-like intracranial aneurysms. Report of a case and review of the literature. Acta Neurochir 148:1091–1095
Banach MJ, Flamm ES (1993) Supraclinoid internal carotid artery fenestration with an associated aneurysm. Case Report J Neurosurg 79:438–441
Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, Moran CJ, Woo HH, Lopes DK, Berez AL, Cher DJ, Siddiqui AH, Levy EI, Albuquerque FC, Fiorella DJ, Berentei Z, Marosfoi M, Cekirge SH, Nelson PK (2013) Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology 267:858–868
Black SP, Ansbacher LE (1984) Saccular aneurysm associated with segmental duplication of the basilar artery. A morphological study. J Neurosurg 61:1005–1008
Chalouhi N, Tjoumakaris S, Starke RM, Gonzalez LF, Randazzo C, Hasan D, McMahon JF, Singhal S, Moukarzel LA, Dumont AS, Rosenwasser R, Jabbour P (2013) Comparison of flow diversion and coiling in large unruptured intracranial saccular aneurysms. Stroke 44:2150–2154
Cruz J, O’Kelly C, Wong JH, Alshaya W, Martin A, Spears J, Marotta TR (2013) Pipeline embolization device in aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol 34:271–276
De Barros FM, Nella Castro R, Lundquist J, Scrivano E, Ceratto R, Ferrario A, Lylyk P (2011) The role of the Pipeline embolization device for the treatment of dissecting intracranial aneurysms. AJNR Am J Neuroradiol 32:2192–2195
Fiorella D, Kelly ME, Albuquerque FC, Nelson PK (2009) Curative reconstruction of a giant midbasilar trunk aneurysm with the Pipeline embolization device. Neurosurgery 64:212–217
Fiorella D, Lylyk P, Szikora I, Kelly ME, Albuquerque FC, McDougall CG, Nelson PK (2009) Curative cerebrovascular reconstruction with the Pipeline embolization device: the emergence of definitive endovascular therapy for intracranial aneurysms. J Neurointerv Surg 1:56–65
Fiorella D, Woo HH, Albuquerque FC, Nelson PK (2008) Definitive reconstruction of circumferential, fusiform intracranial aneurysms with the Pipeline embolization device. Neurosurgery 62:1115–1121
Fischer S, Vajda Z, Perez MA, Schmid M, Hopf N, Bazner H, Henkes H (2012) Pipeline embolization device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology 54:369–382
Ichikawa T, Miyachi S, Izumi T, Matsubara N, Naito T, Haraguchi K, Wakabayashi T, Koketsu N (2011) Fenestration of a supraclinoid internal carotid artery associated with dual aneurysms: case report. Neurosurgery 69:E1005–1009
Inagawa T (2009) Incidence and risk factors for multiple intracranial saccular aneurysms in patients with subarachnoid hemorrhage in Izumo City, Japan. Acta Neurochir 151:1623–1630
Kaminogo M, Yonekura M, Shibata S (2003) Incidence and outcome of multiple intracranial aneurysms in a defined population. Stroke 34:16–21
Kan P, Siddiqui AH, Veznedaroglu E, Liebman KM, Binning MJ, Dumont TM, Ogilvy CS, Gaughen JR Jr, Mocco J, Velat GJ, Ringer AJ, Welch BG, Horowitz MB, Snyder KV, Hopkins LN, Levy EI (2012) Early postmarket results after treatment of intracranial aneurysms with the Pipeline embolization device: a U.S. multicenter experience. Neurosurgery 71:1080–1088
Katsuta T, Matsubara T, Fujii K (1993) Fenestration of the supraclinoid internal carotid artery. Neuroradiology 35:461
Lai LT, Morgan MK, Patel NJ (2014) Smoking increases the risk of de novo intracranial aneurysms. World Neurosurg 82(1–2):e195–201
Li M, Lin N, Wu J, Liang J, He W (2012) Multiple intracranial aneurysms associated with multiple dural arteriovenous fistulas and cerebral arteriovenous malformation. World Neurosurg 77(398):E311–395
Lubicz B, Collignon L, Raphaeli G, J-P P, Bruneau M, De Witte O, Leclerc X (2010) Flow-diverter stent for the endovascular treatment of intracranial aneurysms: a prospective study in 29 patients with 34 aneurysms. Stroke 41:2247–2253
Martin AR, Cruz JP, Matouk CC, Spears J, Marotta TR (2012) The Pipeline flow-diverting stent for exclusion of ruptured intracranial aneurysms with difficult morphologies. Neurosurg (1 Suppl Operative) 70:21–28
McAuliffe W, Wenderoth JD (2012) Immediate and midterm results following treatment of recently ruptured intracranial aneurysms with the Pipeline embolization device. AJNR Am J Neuroradiol 33:487–493
McAuliffe W, Wycoco V, Rice H, Phatouros C, Singh TJ, Wenderoth J (2012) Immediate and midterm results following treatment of unruptured intracranial aneurysms with the Pipeline embolization device. AJNR Am J Neuroradiol 33:164–170
Mut F, Scrivano E, Bleise C, Lylyk P, Cebral J (2013) Hemodynamics in two tandem aneurysms treated with flow diverters. Int J Numer Method Biomed Eng 30:517–524
Narata AP, Yilmaz H, Schaller K, Lovblad KO, Pereira VM (2012) Flow-diverting stent for ruptured intracranial dissecting aneurysm of vertebral artery. Neurosurgery 70:982–989
Nekrysh SY (2000) Association between heritable connective tissue disorders and intracranial aneurysms. Surg Neurol 54:77–78
Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D (2011) The Pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol 32:34–40
Ng PP, Steinfort B, Stoodley MA (2006) Internal carotid artery fenestration with dual aneurysms. Case Illustration. J Neurosurg 104:979
Ogilvy CS, Natarajan SK, Jahshan S, Karmon Y, Yang X, Snyder KV, Hopkins LN, Siddiqui AH, Levy EI (2011) Stent-assisted coiling of paraclinoid aneurysms: risks and effectiveness. J Neurointerv Surg 3:14–20
Ostergaard JR, Hog E (1985) Incidence of multiple intracranial aneurysms. Influence of arterial hypertension and gender. J Neurosurg 63:49–55
Rhoton AL Jr (2002) The supratentorial arteries. Neurosurgery 51:S53–120
Roy D, Milot G, Raymond J (2001) Endovascular treatment of unruptured aneurysms. Stroke 32:1998–2004
Schievink WI (1997) Genetics of intracranial aneurysms. Neurosurgery 40:651–663
Szikora I, Berentei Z, Kulcsar Z, Marosfoi M, Vajda ZS, Lee W, Berez A, Nelson PK (2010) Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the Pipeline embolization device. AJNR Am J Neuroradiol 31:1139–1147
Watnick T, Phakdeekitcharoen B, Johnson A, Gandolph M, Wang M, Briefel G, Klinger KW, Kimberling W, Gabow P, Germino GG (1999) Mutation detection of PKD1 identifies a novel mutation common to three families with aneurysms and/or very-early-onset disease. Am J Hum Genet 65:1561–1571
Wellman BJ, Loftus CM (1998) Bilateral (mirror-image) aneurysms at the origin of the posteroinferior cerebellar artery: case report. Neurosurgery 42:938–940
Acknowledgments
The authors thank Paul H. Dressel BFA for preparation of the illustrations and Debra J. Zimmer for editorial assistance.
Funding statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
Hopkins: grant/research support-Toshiba; consultant-Abbott, Boston Scientific, Cordis, Covidien; financial interests- AccessClosure, Augmenix, Boston Scientific, Claret Medical Inc., Endomation, Ostial Corporation, Silk Road, Valor Medical; board/trustee/officer position-Claret Medical, Inc.; speakers’ bureau-Abbott Vascular; honoraria-Complete Conference Management, Cordis, Covidien, Memorial Healthcare System. Levy: shareholder/ownership interests–Intratech Medical Ltd., Blockade Medical LLC. Principal investigator: Covidien US SWIFT PRIME Trials. Other financial support–Abbott for carotid training for physicians. Mokin: research grant-Toshiba; Siddiqui: research grants (not related to present study)–National Institutes of Health (co-investigator: NINDS 1R01NS064592-01A1 and NIBIB 5 RO1EB002873-07), University at Buffalo (Research Development Award); financial interests–Hotspur, Intratech Medical, StimSox, Valor Medical, Blockade Medical, Lazarus Effect; consultant–Codman & Shurtleff, Inc., Concentric Medical, Covidien Vascular Therapies, GuidePoint Global Consulting, Penumbra, Stryker Neurovascular, Pulsar Vascular; speakers’ bureaus–Codman & Shurtleff, Genentech; National Steering Committees for Penumbra 3D Separator Trial, Covidien SWIFT PRIME Trial, MicroVention FRED Trial; advisory board–Codman & Shurtleff, Covidien Vascular Therapies; honoraria–Abbott Vascular and Codman & Shurtleff, Inc. for training other neurointerventionists in carotid stenting and for training physicians in endovascular stenting for aneurysms. Snyder: research and consultant support-Boston Scientific, Cordis, EndoTex, EPI, Guidant, Medtronic, Micrus, Kerberos, Zimmer, Abbott Vascular, ev3, Toshiba. financial/shareholder interests-EndoTex, Micrus, BSC EPI, Access Closure Inc, Primus, Cordis, Boston Scientific, Niagara Gorge Medical. Xiang: American Society for Quality Biomedical Division Dr. Richard J. Schlesinger grant. No disclosures: Brouillard, Krishna, Lin, Natarajan, Sonig.
Contributorship statement
Lin and Levy are responsible for concepts and design. All authors contributed intellectually. All authors acquired, analyzed, and interpreted the data. Statistical analysis was performed by Lin. Manuscript was prepared by Lin and Brouillard. All authors reviewed and made critical revisions to the manuscript.
Data sharing statement
Additional data from this study (case series) may be made available upon request directed to the corresponding author.
Ethics approval
This study was approved by the University at Buffalo Institutional Review Board (Project 578913-2).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, N., Brouillard, A.M., Xiang, J. et al. Endovascular management of adjacent tandem intracranial aneurysms: Utilization of stent-assisted coiling and flow diversion. Acta Neurochir 157, 379–387 (2015). https://doi.org/10.1007/s00701-014-2318-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2318-z