Abstract
Background
Postoperative cerebral hyperperfusion (HP) is a notable complication that occurs more frequently in moyamoya disease (MMD) than in atherosclerosis. This study aimed to clarify the characteristics of intraoperative indocyanine green (ICG) videoangiography in MMD and atherosclerotic disease in terms of postoperative HP.
Methods
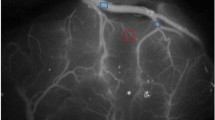
This prospective study included 47 patients with 60 sides that underwent superior temporal artery (STA)-middle cerebral artery (MCA) single bypass. ICG videoangiography was performed after revascularization. The ICG time intensity curve was recorded in the STA, proximal MCA, distal MCA, and superficial Sylvian vein, and the angiographic differences among adult MMD, pediatric MMD, and atherosclerosis were analyzed.
Results
Twenty-two patients (27 sides) had adult MMD, 14 patients (22 sides) had pediatric MMD, and 11 patients (11 sides) had atherosclerosis. Postoperative HP was significantly higher in adult MMD (40.7 %) than in pediatric MMD (18.2 %) and atherosclerosis (0 %). Adult MMD with HP was associated with a longer ICG peak time (P < 0.001). There was no correlation between the ICG peak time and preoperative cerebral blood flow or vascular reserve. The ratio of the vessel caliber was also higher in adult MMD with HP (P < 0.001).
Conclusions
ICG videoangiography provides different characteristics of bypass flow among adult MMD, pediatric MMD, and atherosclerosis. Poor run-off and stagnation of blood flow from the STA might contribute to postoperative HP in MMD. The occurrence of postoperative HP in MMD could depend on two factors: donor STA size and poor run-off and integrity of the blood brain barrier in the recipient MCA.





Similar content being viewed by others
References
Awano T, Sakatani K, Yokose N, Kondo Y, Igarashi T, Hoshino T, Nakamura S, Fujiwara N, Murata Y, Katayama Y, Shikayama T, Miwa M (2010) Intraoperative EC-IC bypass blood flow assessment with indocyanine green angiography in moyamoya and non-moyamoya ischemic stroke. World Neurosurg 73:668–674
Carlson AP, Yonas H, Chang YF, Nemoto EM (2011) Failure of cerebral hemodynamic selection in general or of specific positron emission tomography methodology?: Carotid Occlusion Surgery Study (COSS). Stroke 42:3637–3639
Czabanka M, Pena-Tapia P, Schubert GA, Woitzik J, Horn P, Schmiedek P, Vajkoczy P (2009) Clinical implications of cortical microvasculature in adult Moyamoya disease. J Cereb Blood Flow Metab 29:1383–1387
Czabanka M, Pena-Tapia P, Schubert GA, Woitzik J, Vajkoczy P, Schmiedek P (2008) Characterization of cortical microvascularization in adult moyamoya disease. Stroke 39:1703–1709
Fujimura M, Inoue T, Shimizu H, Saito A, Mugikura S, Tominaga T (2012) Efficacy of prophylactic blood pressure lowering according to a standardized postoperative management protocol to prevent symptomatic cerebral hyperperfusion after direct revascularization surgery for moyamoya disease. Cerebrovasc Dis 33:436–445
Fujimura M, Kaneta T, Mugikura S, Shimizu H, Tominaga T (2007) Temporary neurologic deterioration due to cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in patients with adult-onset moyamoya disease. Surg Neurol 67:273–282
Fujimura M, Mugikura S, Kaneta T, Shimizu H, Tominaga T (2009) Incidence and risk factors for symptomatic cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in patients with moyamoya disease. Surg Neurol 71:442–447
Fujimura M, Shimizu H, Inoue T, Mugikura S, Saito A, Tominaga T (2011) Significance of focal cerebral hyperperfusion as a cause of transient neurologic deterioration after extracranial-intracranial bypass for moyamoya disease: comparative study with non-moyamoya patients using N-isopropyl-p-[(123)I]iodoamphetamine single-photon emission computed tomography. Neurosurgery 68:957–964, discussion 964–955
Fujimura M, Watanabe M, Narisawa A, Shimizu H, Tominaga T (2009) Increased expression of serum Matrix Metalloproteinase-9 in patients with moyamoya disease. Surg Neurol 72:476–480, discussion 480
Fukui M (1997) Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis ('moyamoya' disease). Research Committee on Spontaneous Occlusion of the Circle of Willis (Moyamoya Disease) of the Ministry of Health and Welfare. Jpn Clin Neurol Neurosurg 99(2):S238–S240
Hayashi K, Horie N, Suyama K, Nagata I (2012) Incidence and clinical features of symptomatic cerebral hyperperfusion syndrome after vascular reconstruction. World Neurosurg 78:447–454
Horie N, Morikawa M, Nozaki A, Hayashi K, Suyama K, Nagata I (2011) "Brush Sign" on susceptibility-weighted MR imaging indicates the severity of moyamoya disease. AJNR Am J Neuroradiol 32:1697–1702
Horie N, So G, Debata A, Hayashi K, Morikawa M, Suyama K, Nagata I (2012) Intra-arterial indocyanine green angiography in the management of spinal arteriovenous fistulae: technical case reports. Spine 37:E264–E267
Kaku Y, Iihara K, Nakajima N, Kataoka H, Fukuda K, Masuoka J, Fukushima K, Iida H, Hashimoto N (2012) Cerebral blood flow and metabolism of hyperperfusion after cerebral revascularization in patients with moyamoya disease. J Cereb Blood Flow Metab 32:2066–2075
Kamp MA, Slotty P, Turowski B, Etminan N, Steiger HJ, Hanggi D, Stummer W (2012) Microscope-integrated quantitative analysis of intraoperative indocyanine green fluorescence angiography for blood flow assessment: first experience in 30 patients. Neurosurgery 70:65–73, discussion 73–64
Kang HS, Kim JH, Phi JH, Kim YY, Kim JE, Wang KC, Cho BK, Kim SK (2010) Plasma matrix metalloproteinases, cytokines and angiogenic factors in moyamoya disease. J Neurol Neurosurg Psychiatry 81:673–678
Kawamata T, Kawashima A, Yamaguchi K, Hori T, Okada Y (2011) Usefulness of intraoperative laser Doppler flowmetry and thermography to predict a risk of postoperative hyperperfusion after superficial temporal artery-middle cerebral artery bypass for moyamoya disease. Neurosurg Rev 34:355–362, discussion 362
Kim JE, Oh CW, Kwon OK, Park SQ, Kim SE, Kim YK (2008) Transient hyperperfusion after superficial temporal artery/middle cerebral artery bypass surgery as a possible cause of postoperative transient neurological deterioration. Cerebrovasc Dis 25:580–586
Kuroda S, Houkin K (2008) Moyamoya disease: current concepts and future perspectives. Lancet Neurol 7:1056–1066
Lee M, Guzman R, Bell-Stephens T, Steinberg GK (2011) Intraoperative blood flow analysis of direct revascularization procedures in patients with moyamoya disease. J Cereb Blood Flow Metab 31:262–274
Lee M, Zaharchuk G, Guzman R, Achrol A, Bell-Stephens T, Steinberg GK (2009) Quantitative hemodynamic studies in moyamoya disease: a review. Neurosurg Focus 26:E5
Mizumura S, Nakagawara J, Takahashi M, Kumita S, Cho K, Nakajo H, Toba M, Kumazaki T (2004) Three-dimensional display in staging hemodynamic brain ischemia for JET study: objective evaluation using SEE analysis and 3D-SSP display. Ann Nucl Med 18:13–21
Nakagawa A, Fujimura M, Arafune T, Sakuma I, Tominaga T (2009) Clinical implications of intraoperative infrared brain surface monitoring during superficial temporal artery-middle cerebral artery anastomosis in patients with moyamoya disease. J Neurosurg 111:1158–1164
Powers WJ (2012) Letter by Powers Regarding Article, "Failure of cerebral hemodynamic selection in general or of specific positron emission tomography methodology? Carotid occlusion surgery study (COSS)". Stroke 43:e43, author reply e44
Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP, Investigators C (2011) Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA 306:1983–1992
Raabe A, Beck J, Gerlach R, Zimmermann M, Seifert V (2003) Near-infrared indocyanine green video angiography: a new method for intraoperative assessment of vascular flow. Neurosurgery 52:132–139, discussion 139
Raabe A, Nakaji P, Beck J, Kim LJ, Hsu FP, Kamerman JD, Seifert V, Spetzler RF (2005) Prospective evaluation of surgical microscope-integrated intraoperative near-infrared indocyanine green videoangiography during aneurysm surgery. J Neurosurg 103:982–989
Schubert GA, Seiz-Rosenhagen M, Ortler M, Czabanka M, Scheufler KM, Thome C (2012) Cortical indocyanine green videography for quantification of acute hypoperfusion after subarachnoid hemorrhage: a feasibility study. Neurosurgery 71:260–267, discussion ons267-268
Suzuki J, Kodama N (1983) Moyamoya disease–a review. Stroke 14:104–109
Suzuki J, Takaku A (1969) Cerebrovascular "moyamoya" disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Takagi Y, Sawamura K, Hashimoto N, Miyamoto S (2012) Evaluation of serial intraoperative surgical microscope-integrated intraoperative near-infrared indocyanine green videoangiography in patients with cerebral arteriovenous malformations. Neurosurgery 70:34–42, discussion 42–33
Terborg C, Groschel K, Petrovitch A, Ringer T, Schnaudigel S, Witte OW, Kastrup A (2009) Noninvasive assessment of cerebral perfusion and oxygenation in acute ischemic stroke by near-infrared spectroscopy. Eur Neurol 62:338–343
Uchino H, Kuroda S, Hirata K, Shiga T, Houkin K, Tamaki N (2012) Predictors and clinical features of postoperative hyperperfusion after surgical revascularization for moyamoya disease: a serial single photon emission CT/positron emission tomography study. Stroke 43:2610–2616
Uchino H, Nakamura T, Houkin K, Murata J, Saito H, Kuroda S (2013) Semiquantitative analysis of indocyanine green videoangiography for cortical perfusion assessment in superficial temporal artery to middle cerebral artery anastomosis. Acta Neurochir 155:599–605
Washington CW, Zipfel GJ, Chicoine MR, Derdeyn CP, Rich KM, Moran CJ, Cross DT, Dacey RG Jr (2013) Comparing indocyanine green videoangiography to the gold standard of intraoperative digital subtraction angiography used in aneurysm surgery. J Neurosurg 118:420–427
Yoshimoto T, Houkin K, Kuroda S, Abe H, Kashiwaba T (1997) Low cerebral blood flow and perfusion reserve induce hyperperfusion after surgical revascularization: case reports and analysis of cerebral hemodynamics. Surg Neurol 48:132–138, discussion 138–139
Conflicts of interest
This work was supported in part by a Grant-in-Aid for Scientific Research to N.H. (23791611) and I.N. (24592134). The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horie, N., Fukuda, Y., Izumo, T. et al. Indocyanine green videoangiography for assessment of postoperative hyperperfusion in moyamoya disease. Acta Neurochir 156, 919–926 (2014). https://doi.org/10.1007/s00701-014-2054-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2054-4