Abstract
Background
The angioarchitecture of arteriovenous fistulas (AVFs) of cerebral arteriovenous malformation (CAVM) after stereotactic radiosurgery (SRS) remain unclear. The purpose of this study is to report the angiographic change of AVF components of CAVMs after SRS and outcomes of endovascular embolisation.
Methods
From 2002 to 2012, a total of 523 CAVMs had been treated primarily by SRS with more than 3-year latency. Among these databases, there were 19 patients with 21 AVFs undergoing embolization after SRS. We retrospectively analyzed the angioarchitecture of the CAVM to identify AVFs, morphologic change and outcomes of AVFs after SRS and embolisation.
Results
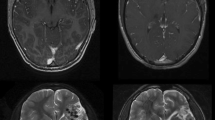
Eight AVFs were in the periphery of CAVMs, the other 13 were in a central location. Eighteen of 21 AVFs remained constant in morphology after SRS, while three feeders of AVFs were associated with radiation arteritis. The causes of failure to identify AVFs before SRS were overlooked (n = 7) or there was superimposition with feeders, nidus and/or venous drains of CAVMs (n = 14). Total fistula occlusion was achieved in all 21 AVFs; residual CAVMs was totally obliterated by embolisation and/or additional SRS in 12 patients. One patient had a small procedure-related intracerebral hemorrhage. Mean follow-up period was 26 months.
Conclusions
Early detection of AVF components of CAVMs prior to SRS may be difficult, particularly those in a central location. However, most AVFs became evident and showed consistency in angiographic morphology after obliteration of the majority nidus parts of CAVMs. Endovascular embolisation is effective in managing these AVF components.



Similar content being viewed by others
References
Chung WY (2009) Radiosurgery for arteriovenous malformation in eloquent region of the brain. Neurol India 57:525–527
Chung WY, Shiau CY, Wu HM, Liu KD, Guo WY, Wang LW, Pan DH (2008) Staged radiosurgery for extra-large cerebral arteriovenous malformations: Method, implementation, and results. J Neurosurg 109:65–72
Cognard C, Spelle L, Peirot (2008) Pial arteriovenous malformations. In: Forsting M, Wanke I (eds) Intracranial vascular malformations and aneurysms. Springer, Heidelberg, pp 51–120
Dawson RC III, Tarr RW, Hecht ST, Jungreis CA, Lunsford LD, Coffey R, Horton JA (1990) Treatment of arteriovenous malformation of the brain with combined embolisation and stereotactic radiosurgery: results after 1 and 2 years. Am J Neuroradiol 11:857–864
Debrun G, Vinuela FV, Fox AJ, Drake CG (1982) Embolisation of cerebral arteriovenous malformations with bucrylate: experience in 46 cases. J Neurosurg 56:615–27
Fournier D, TerBrugge KG, Willinsky R, Lasjaunias P, Montanera W (1991) Endovascular treatment of intracerebral arteriovenous malformation: experience in 49 cases. J Neurosurg 75:228–33
Gallina P, Merienne L, Meder JF, Scholinenger M, Lefkopoulos D, Merland JJ (1998) Failure in radiosurgery treatment of cerebral arteriovenous malformation. Neurosurgery 42:996–1004
Guo WY, Wikholm G, Karlsson B, Lindquist C, Svendsen R, Ericson K (1993) Combined embolisation and gamma knife radiosurgery for cerebral arteriovenous malformations. Acta Radiol 34:600–606
Katsaridis V, Papagiannaki C, Aimar E (2008) Curative embolization of cerebral arteriovenous malformations (AVMs) with Onyx in 101 patients. Neuroradiology 50:589–597
Luo CB, Guo WY, Teng MMH, Chang FC, Lin CJ, Wu HM, Chung WY, Chang CY (2013) Fistula components of brain arteriovenous malformations: angioarchitecture analysis and embolisation prior to Gamma-Knife surgery. J Chin Med Assoc 76:277–281
Luo CB, Guo WY, Teng MM, Chang FC, Pan DH (2005) Embolisation of arteriovenous fistula after radiosurgery for multiple cerebral arteriovenous malformations. Kaohsiung J Med Sci 21:571–577
Mounayer C, Hammami N, Piotin M, Spelle L, Bemdorf G, Kessler I (2007) Moret J (2007) Nidal embolization of brain arteriovenous malformations using Onyx in 94 patients. AJNR Am J Neuroradiol 28:518–523
Murugesan C, Saravanan S, Rajkumar J, Prasad J, Banakal S, Muralidhar K (2008) Severe pulmonary oedema following therapeutic embolization with Onyx for cerebral arteriovenous malformation. Neuroradiology 50(5):439–442
Panagiotopoulos V, Gizewski E, Asgari S, Rogel J, Forsting M, Wanke I (2009) Embolization of intracranial arteriovenous malformations with ethylene-vinyl alcohol copolymer (Onyx). AJNR Am J Neuroradiol 30:99–106
Pollock BE, Flickinger JC, Lunsford LD, Bissonette DJ, Kondziolka D (1996) Hemorrhage risk after stereotactic radiosurgery of cerebral arteriovenous malformations. Neurosurgery 38:652–659
Pollock BE, Kondziolka D, Lunsford LD, Bissonette D, Flickinger JC (1996) Repeated stereotactic radiosurgery of arteriovenous malformations: factor associated with incomplete obliteration. Neurosurgery 38:318–324
Pollock BE, Lunsford LD, Flickinger JC, Kondziolka D (1999) The role of embolisation in combination with stereotactic radiosurgery in the management of pial and dural arteriovenous malformation. In: Connors JJ, Wojak JC (eds) Interventional neuroradiology:strategies and practical techniques. Saunders, Philadelphia, pp 267–275
Söderman M, Anderson T, Karlsson B, Wallace MC, Edner G (2003) Management of patients with brain arteriovenous malformations. Eur J Radiol 46:195–205
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65:476–483
Van Rooij WJ, Sluzewski M, Beute GN (2007) Brain AVM embolization with Onyx. Am J Neuroradiol 50:439–442
Wang H, Lv X, Jiang C, Li Y, Wu Z, Xu K (2009) Onyx migration in the endovascular management of intracranial dural arteriovenous fistulas. Interv Neuroradiol 15:301–8
Acknowledgments
Source of support: This work was supported in part by a grant from the Taipei Veterans General Hospital (V98C1-153, V99C1-012) and the National Science Council (97-2314-B-075-062-my2, 99-2314-B-075-045-my2).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The authors hypothesize that a cerebral AVM consists of two independent components which are relevant for occlusion following radiosurgery (RS). One is the nidus and the other one are high flow shunts (HFS) within the AVM which may or may not be present. They further hypothesize that the response rate to RS is different for the nidus and for HFS with HFS being more radioresistant. The literature on this topic is controversial (1, 2).
Naturally, all AVMs consist of a nidus. Only a fraction of AVMs contain HFS in addition. The percentage of AVMs containing HFS undergoing RS has been reported to be 38.5 % (3). If the authors’ hypothesis is true and considering that occlusion rates for AVMs following RS are about 80 %, the percentage of non-responding HFS cannot be high. This is supported by this study’s finding that only 4 % of AVMs required embolization for the HFS component following RS.
Based on their study, the authors recommend for a number of reasons the following concept in the treatment for cerebral AVMs: deliver RS to the nidus which may or may not contain HFS and for the small percentage of AVMs with non-responding HFS embolize the HFS following RS as opposed to prior to RS. This is an interesting and novel approach for which this study may serve as a proof-of-concept.
1) Kwon Y, Jeon SR, Kim JH, Lee JK, Ra DS, Lee DJ, Kwun BD (2000) Analysis of the causes of treatment failure in gamma knife radiosurgery for intracranial arteriovenous malformations. J Neurosurg 93(Suppl 3):104-106
2) Nagaraja S, Lee KJ, Coley SC, Capener D, Walton L, Kemeny AA, Wilkinson ID, Griffiths PD (2006) Stereotactic radiosurgery for brain arteriovenous malformations: quantitative MR assessment of nidal response at 1 year and angiographic factors predicting early obliteration. Neuroradiol 48:821-829
3) Yuki I, Kim RH, Duckwiler G, Jahan R, Tateshima S, Gonzalez N, Gorgulho A, Diaz JL, De Salles AA, Vinuela F (2010) Treatment of brain arteriovenous malformations with high-flow arteriovenous fistulas: risk and complications associated with endovascular emolization in multimodality treatment. J Neurosurg 113:715–722
Thomas Mindermann
Zurich,Switzerland
Rights and permissions
About this article
Cite this article
Luo, CB., Guo, WY., Chang, FC. et al. Fistula component of cerebral arteriovenous malformations: morphologic change after stereotactic radiosurgery and outcome of embolisation. Acta Neurochir 156, 85–92 (2014). https://doi.org/10.1007/s00701-013-1939-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1939-y