Abstract
Background
The purpose of this study was to evaluate bilateral open-door cervical laminoplasty for management of cervical canal stenosis secondary to multisegmental cervical spondylosis and ossified posterior longitudinal ligament. The importance of unilateral posterior approach with preservation of posterior supporting element is emphasized.
Methods
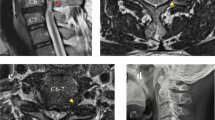
Thirty-four patients had expansive laminoplasty. Posterior tension band consisting of nuchal ligaments and supraspinous and interspinous ligaments was secured. Paraspinal deep extensor muscles attached to one side of spinous process were also preserved. Hydroxyapatite–collagen spacers were positioned between split laminae in midline and secured with Ethibond. All patients had features of myelopathy with weakness, hypertonia, clonus, and hyperreflexia in both upper and lower limbs. Bladder and bowel involvement was seen in 11.7% and sexual dysfunction in 5.8%. Preoperative dynamic study of cervical spine, MRI, and/or CT were done in all patients and compared with postoperative studies to see the efficacy of the surgical procedure.
Results
Preoperative and postoperative neurosurgical cervical spine scale was used to compare results in relation to age, sex, duration of symptoms, neurosurgical cervical spine score, bladder, bowel, and sexual abnormalities. Elderly patients, lower neurosurgical score, signs and symptoms of more than 2 years, and bladder, bowel, and sexual dysfunction had poorer outcome. Complications were few. All patients had adequate diameter of spinal canal postoperatively. Cervical alignment and range of motion of segment subjected to laminoplasty were preserved satisfactorily in follow-up.
Conclusions
Bilateral open-door expansive laminoplasty using unilateral posterior midline approach provides preservation of posterior supporting tension band and excellent reconstruction of spinal canal. This technique also does not compromise contralateral paraspinal muscles attached to spinous process.






Similar content being viewed by others
References
Asgari S, Bassiouni H, Massond N, Schlamann M, Stolke D (2009) Decompressive laminoplasty in multisegmental cervical spondylotic myelopathy: bilateral cutting versus open door technique. Acta Neurochir 151:739–749
Fujita K, Tsuji N, Nishimura Y (1998) Surgical results of the double door laminoplasty splitting the spinous processes preserving the posterior supporting structures. Spinal Surg 12:293–300
Goel A (1997) Vascularized pedicle laminoplasty. Surg Neurol 48:442–445
Handa Y, Kubota T, Ishii H, Sato K, Tsuchida A, Arai Y (2002) Evaluation of prognostic factors and clinical outcome in elderly patients in whom expansive laminoplasty is performed for cervical myelopathy due to multisegmental spondylotic canal stenosis. A retrospective comparison with younger patients. J Neurosurg 96:173–179
Hidai Y, Ebara S, Kamimura M, Tateiwa Y, Itoh H, Kinoshita T, Takaoka K, Ohatsuka K (1999) Treatment of cervical compressive myelopathy with a new dorsolateral decompressive procedure. J Neurosurg 90(4 Suppl):178–185
Iizuka H, Nakajima T, Iizuka Y, Sorimachi Y, Ara T, Nishinome M, Takagishi K (2007) Cervical malalignment after laminoplasty: relationship to deep extensor musculature of the cervical spine and neurological outcome. J Neurosurg (Spine) 7(6):610–614
Johnson KD, Frierson KE, Keller TS, Cook C, Scheinberg R, Zerwekh J, Meyer L, Sciadini MF (1996) Porous ceramics as bone graft substitutes in long bone defects: a biomechanical, histological, and radiographic analysis. J Orthop Res 14:351–369
Kadoya S (1992) Japanese Society of Spine Surgery: grading and scoring system for neurological function in degenerative cervical spine scale. Neurol Med Chir (Tokyo) 32:40–44
Kaner T, Sasani M, Oktenoglu T, Ozer AF (2009) Clinical outcome following cervical laminoplasty for 19 patients with cervical spondylotic myelopathy. Turk Neurosurg 19(2):121–126
Kokubun S, Kashimoto O, Tanaka Y (1994) Histological verification of bone bonding and ingrowth into porous hydroxyapatite spinous process spacer for cervical laminoplasty. Tohoku J Exp Med 173:337–344
Kotani Y, Abumi K, Ito M, Sudo H, Takahata M, Ohshima S (2009) Minimum 2-year outcome of cervical laminoplasty with deep extensor muscle preserving approach impact on cervical spine function and quality of life. Eur Spine J 18(5):663–671
Lee TT, Manzano GR, Green BA (1997) Modified open-door cervical expansive laminoplasty for spondylotic myelopathy: operative technique, outcome and predictors for gait improvement. J Neurosurg 86:64–68
Matsuda Y, Shibata T, Oki S (1999) Outcome of surgical treatment for cervical myelopathy in patients more 75 years of age. Spine 24:529–534
Matz PG, Anderson PA, Groff MW, Heary RF, Holly LT, Kaiser MG, Mummaneni PV, Ryken TC, Choudry TF, Vresilovic EJ, Ressnick DK (2009) Cervical laminoplasty for treatment of cervical degenerative myelopathy. J Neurosurg (Spine) 11:157–169
Okada M, Minamide A, Endo T, Yoshida M, Kawakami M, Ando M (2009) A prospective randomized study of clinical outcome in patients with cervical compressive myelopathy treated with open door or French door laminoplasty. Spine 34(11):1119–1126
Ratliff JK, Cooper PR (2003) Cervical laminoplasty: a critical review. J Neurosurg 98:230–238
Satomi NY, Kohno T (1999) Long term follow-up studies of open door expansive laminoplasty for cervical stenotic myelopathy. Spine 24:507–510
Takayasu M, Takagi T, Nishizawa T, Osuka K, Nakajima T, Yoshida J (2002) Bilateral open-door cervical expansive laminoplasty with hydroxyapatite spacers and titanium screws. J Neurosurg (spine 1) 96:22–28
Tani S, Isoshima A, Nagashima Y, Numoto RT, Abe T (2002) Laminoplasty with preservation of posterior cervical elements: surgical technique. Neurosurgery 50:97–102
Terao S, Sobue G, Hashizume Y (1996) Age related changes of the myelinated fibers in the human spinal ventral horn cells with special reference to loss of small neurons in the intermediate zone: a quantitative analysis. Acta Neuropathol 92:109–114
Yang SC, Niu CC, Chen WJ, Wu CH, Yu SW (2008) Open door laminoplasty for multilevel cervical spondylotic myelopathy: good outcome in 12 patients using suture anchor fixation. Acta Orthop 79(1):62–66
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sinha, S., Jagetia, A. Bilateral open-door expansive laminoplasty using unilateral posterior midline approach with preservation of posterior supporting elements for management of cervical myelopathy and radiculomyelopathy—analysis of clinical and radiological outcome and surgical technique. Acta Neurochir 153, 975–984 (2011). https://doi.org/10.1007/s00701-010-0872-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-010-0872-6