Abstract
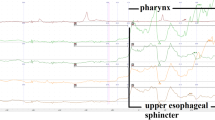
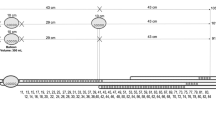
Endoscopic manometry was performed to evaluate the motor activity of the sphincter of Oddi (OS) in six patients with Lemmel’s syndrome, four of whom had acute cholangitis and two of whom had acute pancreatitis. As controls, 24 patients undergoing cholecystectomy without juxtapapillary duodenal diverticula (JPD) for cholelithiasis or cholesterol polyps in the gallbladder were also studied.
The OS basal pressure and contraction pressure values were 12.4±6 5.1mmHg and 103.4±24.3 mmHg, respectively, in the patients with Lemmel’s syndrome, and 19.5±5.1mmHg and 136.8±28.2 mmHg, respectively, in the control patients. These differences between the groups were statistically significant; however, the wave frequency was not significantly different between the groups. The mean percentages of antegrade, simultaneous, and retrograde sequences were 37.5%±11.3%, 19.9%±8.7%, and 43.4%±11.7%, respectively, in the patients with Lemmel’s syndrome, and 66.5% 6 11.0%, 20.2%±4.7%, and 14.3%±9.2%, respectively, in the controls. The differences between the groups were significant (P<0.01) for the antegrade and retrograde sequences. These findings indicate that dysfunction of the OS in patients with Lemmel’s syndrome could be important in the development of hepatocholangiopancreatic disease caused by duodenobiliary and duodenopancreatic reflux.
Similar content being viewed by others
References
Critchlon JF, Shapire ME, Silen W (1985) Duodenojejunostomy for the pancreaticobiliary complications of duodenal diverticulum. Ann Surg 202:56–58
Gudjonsson H, Gamelli RL, Kayc MD (1988) Symptomatic biliary obstruction associated with juxtapapillary duodenal diverticulum. Dig Dis Sci 33:114–121
Tomita R, Nagai N, Aoki N, Tanjoh K, Kurosu Y (1993) Plasma gut hormone levels before and after duodenojejunostomy in patients with juxtapapillary duodenal diverticulum. Biomed Res 14:123–130
Suda K, Mizuguchi K, Matsumoto M (1983) Histopathological study on the etiology of duodenal diverticulum related to the fusion of the pancreatic anlage. Am J Gastroenterol 78:335–338
Viceconte GW, Bogliolo G (1984) Endoscopic manometry of the sphincter of Oddi in patients with and without juxtapapillary duodenal diverticula. Scand J Gastroenterol 19:329–333
Funch-Jensen P (1995) Sphincter of Oddi physiology. J Hepato Biliary Pancreat Surg 2:249–254
Lemmel G (1934) Die Klinische Bedeutung der Duodenaldivertikel. Arch Verdkrht 46:59–70
Meshkinpour H, Mollot M, Eckerling GB, Bookman L (1984) Bile duct dyskinesia. Gastroenterology 87:759–762
Eggert A, Kirschner H, Teichmann W (1979) Bacteriological study in patients with cholelithiasis and duodenal diverticulum. Chirurg 50:441–444
Goldman LD, Steer ML, Silen W (1983) Recurrent cholangitis after biliary surgery. Am J Surg 145:450–454
Miyazaki S, Sakamoto T, Miyata M, Yamasaki Y, Yamasaki H, Kuwata K (1995) Function of the Sphincter of Oddi in patients with juxtapapillary duodenal diverticula: evaluation by intraoperative biliary manometry under a duodenal pressure load. World J Surg 19:307–312
Løtveit T, Skar V, Osnen M (1988) Juxtapapillary duodenal diverticula. Endoscopy 20:175–178
Meshkinpour H, Mollot M, Eckerling GB, Bookman L (1984) Bile duct dyskinesia; clinical and manometric study. Gastroenterology 87:759–762
Coelho JCU, Wiederkehr JC (1996) Motility of Oddi’s sphincter: recent developments and clinical applications. Am J Surg 172:48–51
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tomita, R., Tanjoh, K. Endoscopic manometry of the sphincter of Oddi in patients with Lemmel’s syndrome. Surg Today 28, 258–261 (1998). https://doi.org/10.1007/s005950050117
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s005950050117