Abstract
Purpose
Stoma construction and closure are common surgical strategies in patients with colorectal cancer. The present study evaluated the influence of multiple incisional sites resulting from stoma closure on incisional hernia after colorectal cancer surgery.
Methods
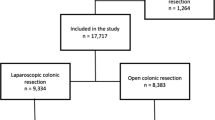
The study included 1681 patients who underwent colorectal cancer surgery. Multiple incisional sites were defined as the coexistence of incisions at the midline and stoma closure sites. We retrospectively investigated the relationship between the presence of multiple incisional sites and incisional hernia development in patients with colorectal cancer.
Results
Among the 1681 patients, 420 (25%) underwent stoma construction, with a stoma closure-to-construction ratio of 33% (139/420), and 155 (9.2%) developed incisional hernias after colorectal cancer surgery. In the multivariate analysis, female sex (p < 0.001), body mass index (p < 0.001), multiple incisional sites (p = 0.001), wound infection (p = 0.003), and postoperative chemotherapy (p = 0.030) were independent predictors of incisional hernia. In the multiple incisional sites group, the age (p < 0.001), surgical approach (laparoscopic) (p = 0.013), wound infection rate (p = 0.046), small bowel obstruction rate (p < 0.001), and anastomotic leakage rate (p = 0.008) were higher in those in the single incisional site group.
Conclusions
Multiple incisional sites resulting from stoma closure are associated with the development of incisional hernia following colorectal cancer surgery.

Similar content being viewed by others
Abbreviations
- APR:
-
Abdominoperineal resection
- AR:
-
Anterior resection
- ASA-PS:
-
American Society of Anesthesiologists physical status
- BMI:
-
Body mass index
- HO:
-
Hartmann’s operation
- IH:
-
Incisional hernia
- ISR:
-
Intersphincteric resection
- PO:
-
Palliative operation
- TP:
-
Total proctocolectomy
- TPE:
-
Total pelvic exenteration
- RHC:
-
Right hemicolectomy
References
Ando Y, Takahashi A, Fujii M, Hasegawa H, Kimura T, Yamamoto H, et al. Survey regarding gastrointestinal stoma construction and closure in Japan. Ann Gastroenterol Surg. 2022;6:212–26.
Yamada T, Okabayashi K, Hasegawa H, Tsuruta M, Abe Y, Ishida T, et al. Age, preoperative subcutaneous fat area, and open laparotomy are risk factors for incisional hernia following colorectal cancer surgery. Ann Surg Oncol. 2016;23(Suppl 2):S236–41.
Hodgson NC, Malthaner RA, Ostbye T. The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg. 2000;231:436–42.
Burger JW, Lange JF, Halm JA, Kleinrensink GJ, Jeekel H. Incisional hernia: early complication of abdominal surgery. World J Surg. 2005;29:1608–13.
Jensen KK, Krarup PM, Scheike T, Jorgensen LN, Mynster T. Incisional hernias after open versus laparoscopic surgery for colonic cancer: a nationwide cohort study. Surg Endosc. 2016;30:4469–79.
Skipworth JR, Khan Y, Motson RW, Arulampalam TH, Engledow AH. Incisional hernia rates following laparoscopic colorectal resection. Int J Surg. 2010;8:470–3.
Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72:70–1.
Yahchouchy-Chouillard E, Aura T, Picone O, Etienne JC, Fingerhut A. Incisional hernias. I. Related risk factors. Dig Surg. 2003;20:3–9.
Fukuoka H, Watanabe J, Masanori O, Suwa Y, Suwa H, Ishibe A, et al. The risk factors for incisional hernia after laparoscopic colorectal surgery: a multicenter retrospective study at Yokohama Clinical Oncology Group. Surg Endosc. 2021;35:3471–8.
Veld J, Umans D, van Halsema E, Amelung F, Fernandes D, Lee MS, et al. Self-expandable metal stent (SEMS) placement or emergency surgery as palliative treatment for obstructive colorectal cancer: A systematic review and meta-analysis. Crit Rev Oncol Hematol. 2020;155: 103110.
Ahmad NZ, Abbas MH, Khan SU, Parvaiz A. A meta-analysis of the role of diverting ileostomy after rectal cancer surgery. Int J Colorectal Dis. 2021;36:445–55.
Yao H, An Y, Zhang Z. The application of defunctioning stomas after low anterior resection of rectal cancer. Surg Today. 2019;49:451–9.
Kaneko T, Funahashi K, Ushigome M, Kagami S, Goto M, Koda T, et al. Incidence of and risk factors for incisional hernia after closure of temporary ileostomy for colorectal malignancy. Hernia. 2019;23:743–8.
Millbourn D, Wimo A, Israelsson LA. Cost analysis of the use of small stitches when closing midline abdominal incisions. Hernia. 2014;18:775–80.
Saijo F, Tokumura H, Narushima Y, Matsumura N, Sato K, Okazaki Y. The quality of life after laparoscopic ventral and incisional hernia repair with closure and non-closure of fascial defect. Surg Today. 2019;49:942–7.
Sadava EE, Kerman Cabo J, Carballo FH, Bun ME, Rotholtz NA. Incisional hernia after laparoscopic colorectal surgery. Is there any factor associated? Surg Endosc. 2014;28:3421–4.
Jairam AP, Timmermans L, Eker HH, Pierik R, van Klaveren D, Steyerberg EW, et al. Prevention of incisional hernia with prophylactic onlay and sublay mesh reinforcement versus primary suture only in midline laparotomies (PRIMA): 2-year follow-up of a multicentre, double-blind, randomised controlled trial. Lancet. 2017;390:567–76.
Mingoli A, Puggioni A, Sgarzini G, Luciani G, Corzani F, Ciccarone F, et al. Incidence of incisional hernia following emergency abdominal surgery. Ital J Gastroenterol Hepatol. 1999;31:449–53.
Walming S, Angenete E, Block M, Bock D, Gessler B, Haglind E. Retrospective review of risk factors for surgical wound dehiscence and incisional hernia. BMC Surg. 2017;17:19.
Murray BW, Cipher DJ, Pham T, Anthony T. The impact of surgical site infection on the development of incisional hernia and small bowel obstruction in colorectal surgery. Am J Surg. 2011;202:558–60.
Yamamoto M, Takakura Y, Ikeda S, Itamoto T, Urushihara T, Egi H. Visceral obesity is a significant risk factor for incisional hernia after laparoscopic colorectal surgery: a single-center review. Asian J Endosc Surg. 2018;11:373–7.
Söderbäck H, Gunnarsson U, Hellman P, Sandblom G. Incisional hernia after surgery for colorectal cancer: a population-based register study. Int J Colorectal Dis. 2018;33:1411–7.
Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract. 2014;105:141–50.
Monteiro R, Azevedo I. Chronic inflammation in obesity and the metabolic syndrome. Mediators Inflamm. 2010. https://doi.org/10.1155/2010/289645.
Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021;320:C375–91.
Takano Y, Kodera K, Tsukihara S, Takahashi S, Yasunobu K, Kanno H, et al. The impact of sarcobesity on incisional hernia after laparoscopic colorectal cancer surgery. Int J Colorectal Dis. 2023;38:124.
European Society of Coloproctology (ESCP) collaborating group. Association of mechanical bowel preparation with oral antibiotics and anastomotic leak following left sided colorectal resection: an international, multi-centre, prospective audit. Colorectal Dis. 2018;20(Suppl 6):15–32.
Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, et al. Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg. 2014;101:1439–47.
Bucknall TE, Cox PJ, Ellis H. Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. Br Med J (Clin Res Ed). 1982;284:931–3.
Santos DA, Zhang L, Do KA, Bednarski BK, Robinson Ledet C, Limmer A, et al. Chemotherapy and abdominal wall closure technique increase the probability of postoperative ventral incisional hernia in patients with colon cancer. Am Surg. 2023;89:98–107.
Lee L, Abou-Khalil M, Liberman S, Boutros M, Fried GM, Feldman LS. Incidence of incisional hernia in the specimen extraction site for laparoscopic colorectal surgery: systematic review and meta-analysis. Surg Endosc. 2017;31:5083–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Compliance with ethical standards
The authors declare no conflicts of interest. The manuscript was not prepared or funded by any commercial organization. The present study was approved by the Institutional Ethics Committee of Jikei University School of Medicine and conformed to the ethical guidelines of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takada, N., Takano, Y., Okamoto, A. et al. Increased risk of incisional hernia after stoma closure in patients with colorectal cancer. Surg Today (2024). https://doi.org/10.1007/s00595-024-02866-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00595-024-02866-2