Abstract
Purpose
Self-expandable metallic stent (SEMS) placement is widely used as a bridge to surgery (BTS) procedure for obstructive colorectal cancer. However, evidence regarding the optimal interval between SEMS placement and elective surgery is lacking.
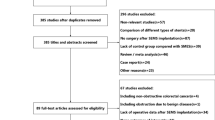
Methods
We retrospectively collected data from patients with BTS between January 2013 and October 2021. Inverse probability treatment-weighted propensity score analyses were used to compare short- and long-term outcomes between the short-interval (SI) and long-interval (LI) groups, using a cutoff of 20 days.
Results
In total, 138 patients were enrolled in this study (SI group, n = 63; LI group, n = 75). In the matched cohort, the patients’ backgrounds were well balanced. The incidence of Clavien–Dindo grade ≥ II postoperative complications was not significantly different between the SI and LI groups (19.0% vs. 14.0%, P = 0.47). There were no significant differences between the SI and LI groups in the 3-year recurrence-free survival (68.0% vs. 76.4%, P = 0.73) or 3-year overall survival rates (86.0% vs. 90.6%, P = 0.72).
Conclusions
A longer interval did not deteriorate the oncological outcomes. Individual perioperative management with an appropriate interval to improve the patient’s condition is required to ensure safe surgery.



Similar content being viewed by others
References
Carraro PGS, Segala M, Cesana BM, Tiberio G. Obstructing colonic cancer: failure and survival patterns over a 10 year follow up after one stage curative surgery. Dis Colon Rectum. 2001;44:243–50.
De Salvo GL, Gava C, Pucciarelli M. Curative surgery for obstruction from primary left colorectal carcinoma: primary or staged resection? Cochrane Database Syst Rev. 2004;2015(2):CD002101.
Manceau G, Voron T, Mege D, Bridoux V, Lakkis Z, Venara A, AFC (French Surgical Association) Working Group, et al. Prognostic factors and patterns of recurrence after emergency management for obstructing colon cancer: multivariate analysis from a series of 2120 patients. Langenbecks Arch Surg. 2019;404:717–29.
Saida Y, Sumiyama Y, Nagao J, Uramatsu M. Long-term prognosis of preoperative “bridge to surgery” expandable metallic stent insertion for obstructive colorectal cancer: comparison with emergency operation. Dis Colon Rectum. 2003;46:S44–9.
Amelung FJ, Draaisma A, Consten ECJ, Siersema PD, ter Borg F. Self-expandable metal stent placement versus emergency resection for malignant proximal colon obstructions. Surg Endosc. 2017;31:4532–41.
Dohmoto M, Rupp KD, Hohlbach G. Endoscopicallyimplanted prosthesis in rectal carcinoma. Dtsch Med Wochenschr. 1990;115:915.
Yang SY, Park YY, Han YD, Cho MS, Hur H, Min BS, et al. Oncologic outcomes of self-expandable metallic stent as a bridge to surgery and safety and feasibility of minimally invasive surgery for acute malignant colonic obstruction. Ann Surg Oncol. 2019;26:2787–96.
Matsuda A, Miyashita M, Matsumoto S, Matsutani T, Sakurazawa N, Takahashi G, et al. Comparison of long-term outcomes of colonic stent as “bridge to surgery” and emergency surgery for malignant large-bowel obstruction: a meta-analysis. Ann Surg Oncol. 2015;22:497–504.
Erichsen R, Horváth-Puhó E, Jacobsen JB, Nilsson T, Baron JA, Sørensen HT. Long-term mortality and recurrence after colorectal cancer surgery with preoperative stenting: a Danish nationwide cohort study. Endoscopy. 2015;47(6):517–24.
Allievi N, Ceresoli M, Fugazzola P, Montori G, Coccolini F, Ansaloni L. Endoscopic stenting as bridge to surgery versus emergency resection for left-sided malignant colorectal obstruction: an updated meta-analysis. Int J Surg Oncol. 2017;2017:2863272.
Matsuda A, Yamada T, Ohta R, Sonoda H, Shinji S, Iwai T, et al. Surgical site infections in gastroenterological surgery. J Nippon Med Sch. 2023;90:2–10.
van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline-Update 2020. Endoscopy. 2020;52:389–407.
Lee GJ, Kim HJ, Baek JH, Lee WS, Kwon KA. Comparison of short-term outcomes after elective surgery following endoscopic stent insertion and emergency surgery for obstructive colorectal cancer. Int J Surg. 2013;11(6):442–6.
Gianotti L, Tamini N, Nespoli L, Rota M, Bolzonaro E, Frego R, et al. A prospective evaluation of short-term and long-term results from colonic stenting for palliation or as a bridge to elective operation versus immediate surgery for large-bowel obstruction. Surg Endosc. 2013;27:832–42.
Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Kawano Y, Yamada T, et al. Optimal interval from placement of a self-expandable metallic stent to surgery in patients with malignant large bowel obstruction: a preliminary study. Surg Laparosc Endosc Percutan Tech. 2018;28:239–44.
Veld JV, Kumcu A, Amelung FJ, Borstlap WAA, Consten ECJ, Dekker JWT, Dutch Snapshot Research Group, et al. Time interval between self-expandable metal stent placement or creation of a decompressing stoma and elective resection of left-sided obstructive colon cancer. Endoscopy. 2021;53:905–13.
Broholm M, Kobborg M, Frostberg E, Jeppesen M, Gögenür I. Delay of surgery after stent placement for resectable malignant colorectal obstruction is associated with higher risk of recurrence. Int J Colorectal Dis. 2017;32:513–6.
Kye BH, Kim JH, Kim HJ, Lee YS, Lee IK, Kang WK, et al. The optimal time interval between the placement of self-expandable metallic stent and elective surgery in patients with obstructive colon cancer. Sci Rep. 2020;10:9502.
Sato R, Oikawa M, Kakita T, Okada T, Abe T, Yazawa T, et al. A longer interval after stenting compromises the short- and long-term outcomes after curative surgery for obstructive colorectal cancer. Surg Today. 2022;52:681–9.
Saito S, Yoshida S, Isayama H, Matsuzawa T, Kuwai T, Maetani I, et al. A prospective multicenter study on self-expandable metallic stents as a bridge to surgery for malignant colorectal obstruction in Japan: efficacy and safety in 312 patients. Surg Endosc. 2016;30:3976–86.
Suzuki M, Okada K, Koyama N, Yamashita N, Yamagishi A, Yamada T, et al. Usefulness of a colonic stent for colonic obstruction caused by lung cancer metastasis. J Nippon Med Sch. 2021;88:556–60.
Hashiguchi Y, Muro K, Saito Y, Hashiguchi Y, Muro K, Saito Y, et al. Japanese Society for Cancer of the Colon and Rectum. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1–42.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36.
Dindo D. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34:3661–79.
Cole SR, Hernán MA. Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed. 2004;75:45–9.
Cwikiel W, Andrén-Sandberg A. Malignant stricture with colovesical fistula: stent insertion in the colon. Radiology. 1993;186:563–4.
Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C, et al. Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol. 2013;22:14–21.
Takahashi G, Yamada T, Iwai T, Takeda K, Koizumi M, Shinji S, et al. Oncological assessment of stent placement for obstructive colorectal cancer from circulating cell-free DNA and circulating tumor DNA dynamics. Ann Surg Oncol. 2018;25:737–44.
Saida Y. Current status of colonic stent for obstructive colorectal cancer in Japan; a review of the literature. J Anus Rectum Colon. 2019;3:99–105.
Ho MF, Futaba K, Chu S, Hon SSF, Ng SSM. Delaying surgery for optimization after colonic stent bridging is safe for left-sided malignant large bowel obstruction: result from 10-year experience and risks factor analysis. Surg Oncol. 2023;47: 101918.
de Roos MAJ, Hugen N, Hazebroek EJ, Bilgen EJS. Delayed surgical resection of primary left-sided obstructing colon cancer is associated with improved short- and long-term outcomes. J Surg Oncol. 2021;124:1146–53.
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg. 2015;261:497–505.
Law WL, Choi HK, Lee YM, Ho JW. The impact of postoperative complications on long-term outcomes following curative resection for colorectal cancer. Ann Surg Oncol. 2007;14:2559–66.
Alonso S, Pascual M, Salvans S, Mayol X, Mojal S, Gil MJ, et al. Postoperative intra-abdominal infection and colorectal cancer recurrence: a prospective matched cohort study of inflammatory and angiogenic responses as mechanisms involved in this association. Eur J Surg Oncol. 2015;41:208–14.
Salvans S, Mayol X, Alonso S, Messeguer R, Pascual M, Mojal S, et al. Postoperative peritoneal infection enhances migration and invasion capacities of tumor cells in vitro: an insight into the association between anastomotic leak and recurrence after surgery for colorectal cancer. Ann Surg. 2014;260:939–43; discussion 943–4.
Tevis SE, Kohlnhofer BM, Stringfield S, Foley EF, Harms BA, Heise CP, et al. Postoperative complications in patients with rectal cancer are associated with delays in chemotherapy that lead to worse disease-free and overall survival. Dis Colon Rectum. 2013;56:1339–48.
Matsuda A, Yamada T, Takahashi G, Matsumoto S, Yokoyama Y, Sonoda H, et al. Postoperative infectious complications have a negative oncological impact in patients after stent placement with malignant large bowel obstruction. Int J Colorectal Dis. 2023;38:2.
Choi MH, Oh SN, Lee IK, Oh ST, Won DD. Sarcopenia is negatively associated with long-term outcomes in locally advanced rectal cancer. J Cachexia Sarcopenia Muscle. 2018;9:53–9.
Kanazawa Y, Yamada T, Kakinuma D, Matsuno K, Ando F, Fujita I, et al. Skeletal muscle mass depletion after gastrectomy negatively affects the prognosis of patients with gastric cancer. Anticancer Res. 2020;40:4271–9.
Sonoda H, Yamada T, Matsuda A, Yokoyama Y, Ohta R, Shinji S, et al. The T-CEA score: a useful prognostic indicator based on postoperative CEA and pathological T4 levels for patients with stage II-III colorectal cancer. Surg Today. 2023;53:890–8.
Han JG, Wang ZJ, Zeng WG, Wang YB, Wei GH, Zhai ZW, et al. Efficacy and safety of self-expanding metallic stent placement followed by neoadjuvant chemotherapy and scheduled surgery for treatment of obstructing left-sided colonic cancer. BMC Cancer. 2020;20:57.
Acknowledgements
We thank Kelly Zammit, BVSc, from Edanz (https://jp.edanz.com/ac) for editing this manuscript.
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
All authors agree with the content of the manuscript. Authors’ contributions are study concept and design; AM and TY, acquisition of data; YY, SM, GT, HS, RO, KU, SS, TI, KT, KS, SK, and TM; analysis and interpretation of data; KS, AM, and YT, drafting of the manuscript; KS and AM, study supervision; TY and HY.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kanaka, S., Matsuda, A., Yamada, T. et al. Oncologic investigation of the interval from stent placement to surgery in patients with obstructive colorectal cancer. Surg Today (2024). https://doi.org/10.1007/s00595-024-02818-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00595-024-02818-w