Abstract
Purpose
To investigate the association between perioperative deglutition screening and postoperative respiratory complications (PRCs) in elderly patients undergoing gastrectomy for gastric cancer.
Methods
We analyzed data from 86 patients with gastric cancer (aged ≥ 70 years) who underwent gastrectomy between October, 2016 and November, 2018. Videofluoroscopic swallowing examinations (VFSEs) were performed before and after surgery. We examined the association of these results with postoperative respiratory complications, as well as the relationships between demographic, operative, and swallowing function assessment data.
Results
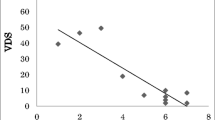
PRCs were identified in 16 patients. The results of pre- and postoperative VFSE showed abnormalities in 28 and 32 patients, respectively. Multivariate analysis revealed that abnormalities in the postoperative VFSEs were strongly associated with the development of PRCs (P = 0.002). The findings of this analysis suggests that ventilatory impairment, a Charlson comorbidity index score ≥ 3, and an open surgical approach are independent risk factors for PRCs.
Conclusion
This is the first study to demonstrate the efficacy of perioperative assessment of swallowing function using VFSE for predicting PRCs in elderly patients undergoing gastrectomy for gastric cancer.
Similar content being viewed by others
References
Suda K, Nakauchi M, Inaba K, Ishida Y, Uyama I. Minimally invasive surgery for upper gastrointestinal cancer: our experience and review of the literature. World J Gastroenterol. 2016;22:4626–37.
Shibata C, Ogawa H, Nakano T, Koyama K, Yamamoto K, Nagao M, et al. Influence of age on postoperative complications especially pneumonia after gastrectomy for gastric cancer. BMC Surg. 2019;19:106.
Yamada H, Shinohara T, Takeshita M, Umesaki T, Fujimori Y, Yamagishi K. Postoperative complications in the oldest old gastric cancer patients. Int J Surg. 2013;11:467–71.
Lawrence VA, Hilsenbeck SG, Mulrow CD, Dhanda R, Sapp J, Page CP. Incidence and hospital stay for cardiac and pulmonary complications after abdominal surgery. J Gen Intern Med. 1995;10:671–8.
Thompson DA, Makary MA, Dorman T, Pronovost PJ. Clinical and economic outcomes of hospital acquired pneumonia in intra-abdominal surgery patients. Ann Surg. 2006;243:547–52.
Hayashi T, Yoshikawa T, Aoyama T, Hasegawa S, Yamada T, Tsuchida K, et al. Impact of infectious complications on gastric cancer recurrence. Gastric Cancer. 2015;18:368–74.
Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Terashima M. Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann Surg Oncol. 2013;20:1575–83.
Gleeson DCL. Oropharyngeal swallowing and aging: a review. J Commun Disord. 1999;32:373–96.
Feng X, Todd T, Lintzenich CR, Ding J, Carr JJ, Ge Y, et al. Aging-related geniohyoid muscle atrophy is related to aspiration status in healthy older adults. J Gerontol A Biol Sci Med Sci. 2013;68:853–60.
Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Motoori M, Fujitani K, Sugimura K, Miyata H, Nakatsuka R, Nishizawa Y, et al. Skeletal muscle loss during neoadjuvant chemotherapy is an independent risk factor for postoperative infectious complications in patients with advanced esophageal cancer. Oncology. 2018;95:281–7.
Eisbruch A, Lyden T, Bradford CR, Dawson LA, Haxer MJ, Miller AE, et al. Objective assessment of swallowing dysfunction and aspiration after radiation concurrent with chemotherapy for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2002;53:23–8.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Weinstock MS, McCoy JL, Cangilla K, Shaffer AD, Maguire RC, J Tobey AB, et al. Predictive utility of the penetration-aspiration scale in inter-arytenoid injection augmentation. Laryngoscope. 2021; 131:E1707–13.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Langerman A, MacCracken E, Kasza K, Haraf DJ, Vokes EE, Stenson KM. Aspiration in chemoradiated patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 2007;133:1289–95.
Atkins BZ, Shah AS, Hutcheson KA, Mangum JH, Pappas TN, Harpole DH, et al. Reducing hospital morbidity and mortality following esophagectomy. Ann Thorac Surg. 2004;78:1170–6.
Mafune T, Mikami S, Otsubo T, Saji O, Matsushita T, Enomoto T, et al. An investigation of factors related to food intake ability and swallowing difficulty after surgery for thoracic esophageal cancer. Dysphagia. 2019;34:592–9.
Berry MF, Atkins BZ, Tong BC, Harpole DH, D’Amico TA, Onaitis MW. A comprehensive evaluation for aspiration after esophagectomy reduces the incidence of postoperative pneumonia. J Thorac Cardiovasc Surg. 2010;140:1266–71.
Maeda K, Koga T, Akagi J. Tentative nil per os leads to poor outcomes in older adults with aspiration pneumonia. Clin Nutr. 2016;35:1147–52.
Wakabayashi H, Kishima M, Itoda M, Fujishima I, Kunieda K, Ohno T, et al. Diagnosis and treatment of sarcopenic dysphagia: A scoping review. Dysphagia. 2021;36:523–31.
Hogue CW, Lappas GD, Creswell LL, Ferguson TB, Sample M, Pugh D, et al. Swallowing dysfunction after cardiac operations: Associated adverse outcomes and risk factors including intraoperative transesophageal echocardiography. J Thorac Cardiovasc Surg. 1995;110:517–22.
Harrington OB, Duckworth JK, Starnes CL, White P, Fleming L, Kritchevsky SB, et al. Silent aspiration after coronary artery bypass grafting. Ann Thorac Surg. 1998;65:1599–603.
Wakabayashi H, Takahashi R, Watanabe N, Oritsu H, Shimizu Y. Prevalence of skeletal muscle mass loss and its association with swallowing function after cardiovascular surgery. Nutrition. 2017;38:70–3.
Miki Y, Makuuchi R, Honda S, Tokunaga M, Tanizawa Y, Bando E, et al. Prospective phase II study evaluating the efficacy of swallow ability screening tests and pneumonia prevention using a team approach for elderly patients with gastric cancer. Gastric Cancer. 2018;21:353–9.
Takahashi T, Kaneoka Y, Maeda A, Takayama Y, Aoyama H, Hosoi T, et al. “Preventative program of aspiration pneumoniae” for prevention of postoperative aspiration pneumoniae in elderly patients with gastrointestinal cancer. Japan J Gastroenterol Surg. 2022;55:733–42.
Beck AM, Kjaersgaard A, Hansen T, Poulsen I. Systematic review and evidence based recommendations on texture modified foods and thickened liquids for adults (above 17 years) with oropharyngeal dysphagia—an updated clinical guideline. Clin Nutr. 2018;37:1980–91.
Miki Y, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Kawamura T, et al. Risk factors for postoperative pneumonia after gastrectomy for gastric cancer. Surg Today. 2016;46:552–6.
Inokuchi M, Kojima K, Kato K, Sugita H, Sugihara K. Risk factors for post-operative pulmonary complications after gastrectomy for gastric cancer. Surg Infect (Larchmt). 2014;15:314–21.
Matsuo Y, Nomi T, Hokuto D, Yoshikawa T, Kamitani N, Sho M. Pulmonary complications after laparoscopic liver resection. Surg Endosc. 2021;35:1659–66.
Zheng HL, Lu J, Zheng CH, Li P, Xie JW, Wang J Bin, et al. Short- and long-term outcomes in malnourished patients after laparoscopic or open radical gastrectomy. World J Surg. 2018; 42:195–203.
Long D, Feng Q, Li Z shun, Zhao Y liang, Qian F, Tang B, et al. Laparoscopic versus open gastrectomy for serosa-invasive gastric cancer: a single-center retrospective cohort study. Surgery. 2021; 169:1486–92.
Pei G, Zhou S, Han Y, Liu Z, Xu S. Risk factors for postoperative complications after lung resection for non-small cell lung cancer in elderly patients at a single institution in China. J Thorac Dis. 2014;6:1230–8.
Laporta ML, Kruthiventi SC, Mantilla CB, Johnson RL, Sprung J, Portner ER, et al. Three risk stratification tools and postoperative pneumonia after noncardiothoracic surgery. Am Surg. 2021;87:1207–13.
Kim S, Kim DH, Park SY, Park CH, Kim HS, Choi SK, et al. Association between Charlson comorbidity index and complications of endoscopic resection of gastric neoplasms in elderly patients. BMC Gastroenterol. 2020;20:213.
Kubo Y, Tanaka K, Yamasaki M, Yamashita K, Makino T, Saito T, et al. Influences of the Charlson comorbidity index and nutrition status on prognosis after esophageal cancer surgery. Ann Surg Oncol. 2021;28:7173–82.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–44.
Dezube AR, Bravo-Iñiguez CE, Yelamanchili N, De León LE, Tarascio J, Jaklitsch MT, et al. Risk factors for delirium after esophagectomy. J Surg Oncol. 2020;121:645–53.
Acknowledgements
We declare that no external funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest for this study to declare.
Ethical statement
The protocol for this research project was approved by the Institutional Review Board of Osaka General Medical Center (approval number: 30-S02-003) and conforms to the provisions of the Declaration of Helsinki. Informed consent was obtained from all the participants or their guardians.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hayashi, Y., Motoori, M., Miyazaki, Y. et al. Impact of the perioperative assessment of deglutition on postoperative respiratory complications in elderly patients undergoing gastrectomy for gastric cancer. Surg Today 54, 258–265 (2024). https://doi.org/10.1007/s00595-023-02728-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02728-3