Abstract
Purpose
We evaluated the clinical outcomes and costs of surgical aortic valve replacement (SAVR) and transfemoral transcatheter aortic valve implantation (TAVI) for aortic stenosis using the Japanese Diagnosis Procedure Combination (DPC) database.
Methods
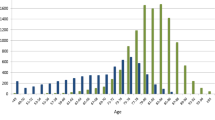
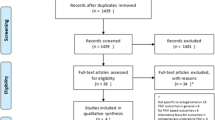
Using our extraction protocol, we retrospectively analyzed summary tables in the DPC database from 2016 to 2019, which were provided by the Ministry of Health, Labor and Welfare. A total of 27,278 patients were available (SAVR, n = 12,534; TAVI, n = 14,744).
Results
The TAVI group was older than the SAVR group (SAVR vs. TAVI: 74.6 vs. 84.5 years; P < 0.01), with a lower in-hospital mortality (1.0 vs. 0.6%; P < 0.01) and a shorter hospital stay (26.9 vs. 20.3 days; P < 0.01). TAVI conferred more total medical service reimbursement points than SAVR (493,944 vs. 605,241 points; P < 0.01), especially materials points (147,830 vs. 434,609 points; P < 0.01). Total insurance claims for TAVI were approximately 1 million yen higher than those for SAVR. Regarding the details of costs, only the operation cost was higher, while other costs were lower with TAVI than with SAVR.
Conclusion
Our analysis revealed that both SAVR and TAVI showed acceptable clinical outcomes. TAVI was associated with higher total insurance claims than SAVR. If the material cost of TAVI operations can be reduced, greater cost-effectiveness can be expected.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the Ministry of Health, Labor and Welfare (MHLW). Restrictions apply to the availability of these data, which were used after passing the screening process for this study. Data are available from the corresponding author with the permission of the MHLW.
References
Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374(17):1609–20.
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019;380(18):1706–15.
Takeji Y, Taniguchi T, Morimoto T, Saito N, Ando K, Shirai S, et al. Transcatheter aortic valve implantation vs. surgical aortic valve replacement for severe aortic stenosis in real-world clinical practice. Circ J. 2020;84(5):806–14.
Kamon T, Kaneko H, Kiriyama H, Itoh H, Fujiu K, Kumazawa R, et al. Transcatheter aortic valve implantation and surgical aortic valve replacement for aortic stenosis in Japan- analysis of a nationwide inpatient database. Circ Rep. 2020;2(12):753–8.
Tabata M, Kumamaru H, Ono A, Miyata H, Sato Y, Motomura N. The association of in-hospital transcatheter aortic valve replacement availability on outcomes of surgical aortic valve replacement in elderly patients. Circ J. 2020;84(9):1599–604.
McCarthy FH, Savino DC, Brown CR, Bavaria JE, Kini V, Spragan DD, et al. Cost and contribution margin of transcatheter versus surgical aortic valve replacement. J Thorac Cardiovasc Surg. 2017;154(6):1872-1880.e1.
Sunner M, Qiu F, Manoragavan R, Roifman I, Tam DY, Fremes SC, et al. Predictors of cumulative cost for patients with severe aortic stenosis referred for surgical or transcatheter aortic valve replacement: a population-based study in Ontario, Canada. Eur Heart J Qual Care Clin Outcomes. 2021;7(3):265–72.
Hayashida K, Murakami G, Matsuda S, Fushimi K. History and profile of diagnosis procedure combination (DPC): development of a real data collection system for acute inpatient care in Japan. J Epidemiol. 2021;31(1):1–11.
Umegaki T, Kunisawa S, Nakajima Y, Kamibayashi T, Fushimi K, Imanaka Y. Comparison of In-hospital outcomes between transcatheter and surgical aortic valve replacement in patients with aortic valve stenosis: a retrospective cohort study using administrative data. J Cardiothorac Vasc Anesth. 2018;32(3):1281–8.
Committee for Scientific Affairs TJAfTS, Shimizu H, Okada M, Toh Y, Doki Y, Endo S, et al. Thoracic and cardiovascular surgeries in Japan during 2018: annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2021;69(1):179–212.
Ando T, Onishi T, Kuno T, Briasoulis A, Takagi H, Grines CL, et al. Transcatheter versus surgical aortic valve replacement in the United States (from the Nationwide Readmission Database). Am J Cardiol. 2021;148:110–5.
Shah KK, Elder D, Nguyen MTH, Turner L, Doyle M, Woldendorp K, et al. Transcatheter aortic valve implantation (TAVI) versus surgical aortic valve replacement for aortic stenosis (SAVR): a cost-comparison study. Heart Lung Circ. 2021;30(12):1918–28.
Kodera S, Kiyosue A, Ando J, Komuro I. Cost effectiveness of transcatheter aortic valve implantation in patients with aortic stenosis in Japan. J Cardiol. 2018;71(3):223–9.
Acknowledgements
We appreciate the support of Professor Chisato Shimanoe from the Department of Pharmacy, Saga University Hospital, Saga, Japan in relation to the statistical methods of the present study.
Funding
This work was supported by JSPS KAKENHI Grant Numbers JP15K08850 and JP18K08764).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Junji Yunoki and other coauthors declare no conflicts of interest in association with the present study.
IRB information
Clinical Research Ethics Review Committee of The Saga University Faculty of Medicine (Reference Number: 2021-01-R-05).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Annual Clinical Outcome and Medical Cost Data
Appendix: Annual Clinical Outcome and Medical Cost Data
SAVR | TAVI | |||||
|---|---|---|---|---|---|---|
FY2016 | FY2017 | FY2018 | FY2016 | FY2017 | FY2018 | |
Number of patients | 4232 | 4303 | 3999 | 3099 | 5068 | 6577 |
Age (years) | 74.8 ± 7.9 | 74.7 ± 8.0 | 74.4 ± 7.8 | 84.4 ± 5.2 | 84.6 ± 5.1 | 84.5 ± 5.2 |
Male sex: n (%) | 1865 (44.1) | 1941 (45.1) | 1871 (46.8) | 990 (31.9) | 1520 (30.0) | 2059 (31.3) |
Preoperative LOS (days) | 5.2 ± 5.6 | 5.2 ± 5.5 | 5.1 ± 5.8 | 7.1 ± 9.7 | 7.2 ± 10.5 | 6.9 ± 9.4 |
Postoperative LOS (days) | 22.1 ± 16.7 | 21.6 ± 15.7 | 21.3 ± 14.7 | 13.5 ± 11.4 | 13.3 ± 12.1 | 13.0 ± 12.3 |
Total LOS (days) | 27.4 ± 18.2 | 26.8 ± 17.4 | 26.4 ± 16.6 | 20.6 ± 16.4 | 20.5 ± 17.8 | 19.9 ± 16.9 |
In-hospital mortality (%) | 1.28 (54/4232) | 0.91 (39/4303) | 0.80 (32/3999) | 0.68 (21/3099) | 0.71 (36/5068) | 0.49 (32/6577) |
Medical service reimbursement points (points) | ||||||
Total | 489,824 ± 206,937 | 494,902 ± 207,874 | 497,272 ± 200,292 | 606,089 ± 207,574 | 607,694 ± 201,745 | 602,952 ± 189,923 |
Drugs | 29,265 ± 36,330 | 29,154 ± 40,711 | 28,578 ± 33,048 | 8,655 ± 18,155 | 7,777 ± 18,167 | 6,661 ± 23,990 |
Materials | 147,646 ± 50,226 | 149,203 ± 52,986 | 146,549 ± 49,954 | 431,636 ± 126,334 | 435,647 ± 116,953 | 435,210 ± 104,490 |
Medical costs (yen) | ||||||
Operation | 3,186,301 ± 649,809 | 3,204,192 ± 732,577 | 3,177,055 ± 684,764 | 5,049,085 ± 926,401 | 5,038,286 ± 904,679 | 4,963,165 ± 902,556 |
Anesthesia | 333,171 ± 193,386 | 331,577 ± 187,550 | 346,005 ± 203,186 | 130,648 ± 232,810 | 132,725 ± 291,217 | 154,039 ± 411,918 |
Injection | 143,846 ± 337,817 | 139,686 ± 353,342 | 120,978 ± 268,055 | 48,995 ± 128,736 | 49,530 ± 176,361 | 41,542 ± 181,882 |
Oral medication | 12,713 ± 23,638 | 12,552 ± 18,431 | 12,638 ± 23,927 | 11,349 ± 20,843 | 11,833 ± 35,620 | 10,724 ± 23,991 |
Clinical examination | 114,426 ± 90,208 | 111,516 ± 85,614 | 109,388 ± 81,291 | 104,683 ± 86,704 | 105,166 ± 85,321 | 106,503 ± 90,616 |
Imaging examination | 49,689 ± 45,061 | 49,078 ± 44,191 | 48,523 ± 41,719 | 51,700 ± 47,492 | 49,068 ± 44,666 | 47,638 ± 47,175 |
Hospitalization | 839,819 ± 475,810 | 847,603 ± 471,824 | 863,965 ± 461,309 | 596,698 ± 429,148 | 585,452 ± 459,306 | 583,972 ± 440,255 |
Continuous data are shown as the mean ± standard deviation.
FY, fiscal year; LOS, length of hospital stay; SAVR, surgical aortic valve replacement; TAVI, transcatheter aortic valve implantation.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yunoki, J., Morita, S., Hayashi, N. et al. The comparison of the clinical outcomes and costs between surgical aortic valve replacement and transcatheter aortic valve implantation based on the Japanese Diagnosis Procedure Combination database. Surg Today 54, 240–246 (2024). https://doi.org/10.1007/s00595-023-02722-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02722-9