Abstract
Purpose
Latent lymph node metastasis is a clinical concern in the surgical treatment of non-small cell lung cancer (NSCLC). The present study identified a simple tool, including the volume-doubling time (VDT), for evaluating the risk of nodal metastasis.
Methods
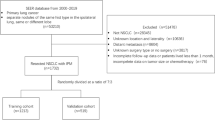
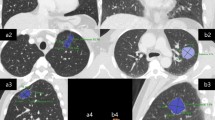
We reviewed, retrospectively, 560 patients who underwent radical resection for cN0M0 NSCLC. The whole tumor VDT and solid component VDT (SVDT) for differentiating the histological type and adenocarcinoma subtype were analyzed and a nomogram was constructed using variables selected through a stepwise selection method. The model was assessed through a calibration curve and decision curve analysis (DCA).
Results
Lymph node metastases were detected in 89 patients (15.9%). The SVDT tended to be longer in patients with adenocarcinoma (294.5 days, p < 0.0001) than in those with other histological types of NSCLC, but was shorter when the solid/micropapillary component was predominant (127.0 days, p < 0.0001). The selected variables (tumor location, solid component diameter, consolidation tumor ratio, SVDT, and carcinoembryonic antigen) demonstrated significant differences and were used for the nomogram. The calibration curve indicated consistency, and the DCA showed validity across most threshold ranges from 0 to 68%.
Conclusions
The established nomogram is a useful tool for the preoperative prediction of lymph node metastasis, and the SVDT was the most influential factor in the nomogram.




Similar content being viewed by others
References
Collaboration GB of DC, Fitzmaurice C, Abate D, Abbasi N, Abbastabar H, Abd-Allah F, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017. Jama Oncol. 2019;5:1749–68.
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WEE, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (Eighth) Edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11:39–51.
National Comprehensive Cancer Network clinical practice guidelines in oncology non-small cell lung cancer. Version 3.2022.
Birim Ö, Kappetein AP, Stijnen T, Bogers AJJC. Meta-analysis of positron emission tomographic and computed tomographic imaging in detecting mediastinal lymph node metastases in non-small cell lung cancer. Ann Thorac Surg. 2005;79:375–82.
Shen G, Lan Y, Zhang K, Ren P, Jia Z. Comparison of 18F-FDG PET/CT and DWI for detection of mediastinal nodal metastasis in non-small cell lung cancer: a meta-analysis. PLoS ONE. 2017;12: e0173104.
Houdu B, Lasnon C, Licaj I, Thomas G, Do P, Guizard A-V, et al. Why harmonization is needed when using FDG PET/CT as a prognosticator: demonstration with EARL-compliant SUV as an independent prognostic factor in lung cancer. Eur J Nucl Med Mol. 2019;I(46):421–8.
Dhopeshwarkar MR, Roberts HC, Paul NS, Dong Z, Tsao M, Menezes RJ. Screen-detected Lung cancer a retrospective analysis of CT appearance. Acad Radiol. 2011;18:1270–6.
Muraoka Y, Yoshida Y, Nakagawa K, Ito K, Watanabe H, Narita T, et al. Maximum standardized uptake value of the primary tumor does not improve candidate selection for sublobar resection. J Thorac Cardiovasc Surg. 2022;163:1656-1665.e3.
Dong X, Qiu X, Liu Q, Jia J. Endobronchial ultrasound-guided transbronchial needle aspiration in the mediastinal staging of non-small cell lung cancer: a meta-analysis. Ann Thorac Surg. 2013;96:1502–7.
Xu DM, Gietema H, de Koning H, Vernhout R, Nackaerts K, Prokop M, et al. Nodule management protocol of the NELSON randomized lung cancer screening trial. Lung Cancer. 2006;54:177–84.
Xu DM, van der Zaag-Loonen HJ, Oudkerk M, Wang Y, Vliegenthart R, Scholten ET, et al. Smooth or attached solid indeterminate nodules detected at baseline CT screening in the NELSON Study: cancer risk during 1 year of follow-up. Radiology. 2009;250:264–72.
Setojima Y, Shimada Y, Tanaka T, Shigefuku S, Makino Y, Maehara S, et al. Prognostic impact of solid-part tumor volume doubling time in patients with radiological part-solid or solid lung cancer. Eur J Cardio-thorac. 2019. https://doi.org/10.1093/ejcts/ezz305.
Miura K, Hamanaka K, Koizumi T, Kawakami S, Kobayashi N, Ito K. Solid component tumor doubling time is a prognostic factor in non-small cell lung cancer patients. J Cardiothorac Surg. 2019;14:57.
Park S, Lee SM, Kim S, Lee J-G, Choi S, Do K-H, et al. Volume doubling times of lung adenocarcinomas: correlation with predominant histologic subtypes and prognosis. Radiology. 2020;295: 191835.
Nakahashi K, Shiono S, Nakatsuka M, Endo M. Prediction of lymph node metastasis of clinical stage IA non-small cell lung cancer based on the tumor volume doubling time. Surg Today. 2022;52:1063–71.
Usuda K, Saito Y, Sagawa M, Sato M, Kanma K, Takahashi S, et al. Tumor doubling time and prognostic assessment of patients with primary lung cancer. Cancer. 1994;74:2239–44.
Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26:565–74.
Moreira AL, Ocampo PSS, Xia Y, Zhong H, Russell PA, Minami Y, et al. A grading system for invasive pulmonary adenocarcinoma: a proposal from the international association for the study of lung cancer pathology committee. J Thorac Oncol. 2020;15:1599–610.
Zhang Y, Sun Y, Xiang J, Zhang Y, Hu H, Chen H. A prediction model for N2 disease in T1 non–small cell lung cancer. J Thorac Cardiovasc Surg. 2012;144:1360–4.
Wang Z, Wu Y, Wang L, Gong L, Han C, Liang N, et al. Predicting occult lymph node metastasis by nomogram in patients with lung adenocarcinoma ≤2 cm. Future Oncol. 2021;17:2005–13.
Kent M, Landreneau R, Mandrekar S, Hillman S, Nichols F, Jones D, et al. Segmentectomy versus wedge resection for non-small cell lung cancer in high-risk operable patients. Ann Thorac Surg. 2013;96:1747–55.
Mokhles S, Macbeth F, Treasure T, Younes RN, Rintoul RC, Fiorentino F, et al. Systematic lymphadenectomy versus sampling of ipsilateral mediastinal lymph-nodes during lobectomy for non-small cell lung cancer: a systematic review of randomized trials and a meta-analysis. Eur J Cardio-thorac. 2017;51:1149–56.
Shimizu K, Yoshida J, Nishimura M, Takamochi K, Nakahara R, Nagai K. Treatment strategy for chylothorax after pulmonary resection and lymph node dissection for lung cancer. J Thorac Cardiovasc Surg. 2002;124:499–502.
Funding
We declare that no funds, grants, or other support was received for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no relevant financial or nonfinancial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
595_2023_2695_MOESM1_ESM.pdf
Supplementary file1 (PDF 145 KB) Supplementary Fig. 1. Nomogram to predict pN2 for patients with cN0M0 lung cancer. A nomogram predicting mediastinal lymph node metastasis in the 560 patients was constructed based on tumor markers and imaging findings. SCD solid component diameter, CTR consolidation tumor ratio, SVDT solid component volume doubling time, CEA carcinoembryonic antigen
595_2023_2695_MOESM2_ESM.pdf
Supplementary file2 (PDF 479 KB) Supplementary Fig. 2. Predictive performance of the nomogram for pN2. a ROC curve for the nomogram for the selected variables and each variable. The area under the ROC curve was 0.795 (95% CI 0.741-0.848). b Calibration curve of the nomogram. The solid line is the bias-corrected curve after 1000 bootstrap sampling iterations. c DCA of the nomogram. DCA showed clinical usefulness with a range of 0% to 26% and 31% to 50%. AUC area under the curve, ROC receiver operating characteristic, DCA decision curve analysis
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karita, R., Suzuki, H., Onozato, Y. et al. A simple nomogram for predicting occult lymph node metastasis of non-small cell lung cancer from preoperative computed tomography findings, including the volume-doubling time. Surg Today 54, 31–40 (2024). https://doi.org/10.1007/s00595-023-02695-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02695-9