Abstract
Purpose
This study aimed to evaluate the learning curve of thoracoscopic repair of tracheoesophageal fistula (TEF) by a single surgeon using a cumulative sum (CUSUM) analysis.
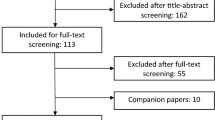
Methods
Prospective clinical data of consecutive Gross type-C TEF repairs performed by a pediatric surgeon from 2010 to 2020 were recorded. CUSUM charts for anastomosis and operating times were generated. The learning curves were compared with the effect of accumulation based on case experience.
Results
For 33 consecutive cases, the mean operative and anastomosis times were 139 ± 39 min and 3137 ± 1110 s, respectively. Significant transitions beyond the learning phase for total operating and anastomosis times were observed at cases 13 and 17. Both the total operating time and anastomosis time were significantly faster in the proficiency improvement phase than in the initial learning phase. Postoperative complications significantly decreased after the initial anastomosis learning phase but not after the initial total operating learning phase.
Conclusions
Thoracoscopic repair of TEF is considered safe and feasible after 13 cases, where the surgeon can improve their proficiency with the total operation procedure, and 17 cases, which will enable the surgeon to achieve proficiency in anastomosis. Postoperative complications significantly decreased after gaining familiarity with the anastomosis procedure through the learning phase.


Similar content being viewed by others
References
Rodgers BM, Talbert JL. Thoracoscopy for diagnosis of intrathoracic lesions in children. J Pediatr Surg. 1976;11:703–8.
Rothenberg SS. Thoracoscopic repair of tracheoesophageal fistula in newborns. J Pediatr Surg. 2002;37:869–72.
Karpelowsky J. Paediatric thoracoscopic surgery. Paediatr Respir Rev. 2012; 13:244–50; quiz 250–41.
Khan N, Abboudi H, Khan MS, Dasgupta P, Ahmed K. Measuring the surgical “learning curve”: methods, variables and competency. BJU Int. 2014;113:504–8.
Biau DJ, Resche-Rigon M, Godiris-Petit G, Nizard RS, Porcher R. Quality control of surgical and interventional procedures: a review of the CUSUM. Qual Saf Health Care. 2007;16:203–7.
Steiner SH, Woodall WH. Debate: what is the best method to monitor surgical performance? BMC Surg. 2016;16:15.
Cundy TP, Gattas NE, White AD, Najmaldin AS. Learning curve evaluation using cumulative summation analysis-a clinical example of pediatric robot-assisted laparoscopic pyeloplasty. J Pediatr Surg. 2015;50:1368–73.
Shirota C, Tanaka Y, Tainaka T, Sumida W, Yokota K, Makita S, et al. Therapeutic strategy for thoracoscopic repair of esophageal atresia and its outcome. Pediatr Surg Int. 2019;35:1071–6.
Novoa NM, Varela G. Monitoring surgical quality: the cumulative sum (CUSUM) approach. Mediastinum. 2020;4:4.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;24:205–13.
Pinheiro PF, Simões e Silva AC, Pereira RM. Current knowledge on esophageal atresia. World J Gastroenterol. 2012; 18(28):3662–72.
Comella A, Tan Tanny SP, Hutson JM, Omari TI, Teague WJ, Nataraja RM, King SK. Esophageal morbidity in patients following repair of esophageal atresia: a systematic review. J Pediatr Surg. 2021;56(9):1555–63.
Tambucci R, Isoldi S, Angelino G, Torroni F, Faraci S, Rea F, et al. Evaluation of gastroesophageal reflux disease 1 year after esophageal atresia repair: paradigms lost from a single snapshot? J Pediatr. 2021;228:155-63.e1.
Al-Qahtani AR, Almaramhi H. Minimal access surgery in neonates and infants. J Pediatr Surg. 2006;41:910–3.
Allal H, Kalfa N, Lopez M, Forgues D, Guibal MP, Raux O, et al. Benefits of the thoracoscopic approach for short- or long-gap esophageal atresia. J Laparoendosc Adv Surg Tech A. 2005;15:673–7.
Drevin G, Andersson B, Svensson JF. Thoracoscopy or thoracotomy for esophageal atresia: a systematic review and meta-analysis. Ann Surg. 2021;274:945–53.
Szavay PO, Zundel S, Blumenstock G, Kirschner HJ, Luithle T, Girisch M, et al. Perioperative outcome of patients with esophageal atresia and tracheo-esophageal fistula undergoing open versus thoracoscopic surgery. J Laparoendosc Adv Surg Tech A. 2011;21:439–43.
van der Zee DC, Tytgat SH, Zwaveling S, van Herwaarden MY, Vieira-Travassos D. Learning curve of thoracoscopic repair of esophageal atresia. World J Surg. 2012;36:2093–7.
Lugo B, Malhotra A, Guner Y, Nguyen T, Ford H, Nguyen NX. Thoracoscopic versus open repair of tracheoesophageal fistula and esophageal atresia. J Laparoendosc Adv Surg Tech A. 2008;18:753–6.
Etchill EW, Giuliano KA, Boss EF, Rhee DS, Kunisaki SM. Association of operative approach with outcomes in neonates with esophageal atresia and tracheoesophageal fistula. J Pediatr Surg. 2021;56:2172–9.
Lee S, Lee SK, Seo JM. Thoracoscopic repair of esophageal atresia with tracheoesophageal fistula: overcoming the learning curve. J Pediatr Surg. 2014;49:1570–2.
Kwak HY, Kim SH, Chae BJ, Song BJ, Jung SS, Bae JS. Learning curve for gasless endoscopic thyroidectomy using the trans-axillary approach: a CUSUM analysis of a single surgeon’s experience. Int J Surg. 2014;12:1273–7.
Wohl H. The CUSUM plot: its utility in the analysis of clinical data. N Engl J Med. 1977;296:1044–5.
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011;25:855–60.
Kim W, Son J, Lee S, Seo JM. The learning curve for thoracoscopic repair of esophageal atresia with distal tracheoesophageal fistula: a cumulative sum analysis. J Pediatr Surg. 2020;55:2527–30.
Funding
This study was supported by JSPS KAKENHI (Grant Number: JP19120733).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
Ethical standards
All procedures performed in this study were per the ethical standards of the institutional and national research committees and the 1964 Declaration of Helsinki and its later amendments. Before the commencement of the study, all protocols were approved by the ethics review board of our institute (Approval number: 2022–0491). This study was approved by the Ethics Committee of our institute.
Research involving human participants
All procedures performed in this study were in accordance with the ethical standards of the Ethics Review Board at Nagoya University Graduate School of Medicine.
Informed consent
As this was a retrospective observational study and the data analyzed were anonymized, informed consent from the participants or their parents/guardians was obtained through an opt-out method on our hospital website in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, Y., Hinoki, A., Deie, K. et al. Anastomotic time was associated with postoperative complications: a cumulative sum analysis of thoracoscopic repair of tracheoesophageal fistula in a single surgeon’s experience. Surg Today 53, 1363–1371 (2023). https://doi.org/10.1007/s00595-023-02687-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02687-9