Abstract
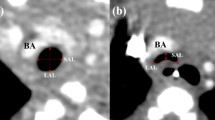
Despite improving the survival after repair of esophageal atresia (EA), the morbidity of EA repair remains high. Specifically, tracheomalacia (TM) is one of the most frequent complications of EA repair. Continuous positive airway pressure is generally applied for the treatment of TM. However, surgical intervention is required against an apparent life-threatening event or inability to perform extubation for a long period. According to our review, most cases of TM showed symptom improvement after aortopexy. The ratio of the trachea’s lateral and anterior–posterior diameter at the brachiocephalic artery crossing the trachea, which reflects the compression of the trachea by the brachiocephalic artery, is a good indicator of aortopexy. Our finding suggests that most TM cases associated with EA may not be caused by tracheal fragility alone, but may involve blood vessel compression. Posterior tracheopexy (PT) is also an effective treatment for TM. Recently, open or thoracoscopic PT was able to be performed simultaneously with EA repair. In many cases, aortopexy or PT is a safe and effective surgical treatment for TM with EA. Other surgical procedures, such as external stenting, should be considered for patients with diffuse-type TM for whom aortopexy and PT appear relatively ineffective.






Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in the published articles in the references.
References
Nassar N, Leoncini E, Amar E, Arteaga-Vazquez J, Bakker MK, Bower C, Canfield MA, Castilla EE, Cocchi G, Correa A, Csaky-Szunyogh M, Feldkamp ML, Khoshnood B, Landau D, Lelong N, Lopez-Camelo JS, Lowry RB, McDonnell R, Merlob P, Metneki J, Morgan M, Mutchinick OM, Palmer MN, Rissmann A, Siffel C, Sipek A, Szabova E, Tucker D, Mastroiacovo P. Prevalence of esophageal atresia among 18 international birth defects surveillance programs. Birth Defects Res A Clin Mol Teratol. 2012;94:893–9. https://doi.org/10.1002/bdra.23067.
Quiroz HJ, Turpin A, Willobee BA, Ferrantella A, Parreco J, Lasko D, Perez EA, Sola JE, Thorson CM. Nationwide analysis of mortality and hospital readmissions in esophageal atresia. J Pediatr Surg. 2020. https://doi.org/10.1016/j.jpedsurg.2020.01.025.
Masuya R, Kaji T, Mukai M, Nakame K, Kawano T, Machigashira S, Yamada W, Yamada K, Onishi S, Yano K, Moriguchi T, Sugita K, Kawano M, Noguchi H, Suzuhigashi M, Muto M, Ieiri S. Predictive factors affecting the prognosis and late complications of 73 consecutive cases of esophageal atresia at 2 centers. Pediatr Surg Int. 2018;34:1027–33. https://doi.org/10.1007/s00383-018-4326-1.
Keefe G, Culbreath K, Edwards EM, Morrow KA, Soll RF, Modi BP, Horbar JD, Jaksic T. Current outcomes of infants with esophageal atresia and tracheoesophageal fistula: a multicenter analysis. J Pediatr Surg. 2022;57:970–4. https://doi.org/10.1016/j.jpedsurg.2022.01.060.
Rayyan M, Embrechts M, Van Veer H, Aerts R, Hoffman I, Proesmans M, Allegaert K, Naulaers G, Rommel N. Neonatal factors predictive for respiratory and gastro-intestinal morbidity after esophageal atresia repair. Pediatr Neonatol. 2019;60:261–9. https://doi.org/10.1016/j.pedneo.2018.07.003.
Engum SA, Grosfeld JL, West KW, Rescorla FJ, Scherer LR 3rd. Analysis of morbidity and mortality in 227 cases of esophageal atresia and/or tracheoesophageal fistula over two decades. Archiv Surg (Chicago Ill: 1960). 1995;130:502–8. https://doi.org/10.1001/archsurg.1995.01430050052008. (discussion 508-509).
DeBoer EM, Prager JD, Ruiz AG, Jensen EL, Deterding RR, Friedlander JA, Soden J. Multidisciplinary care of children with repaired esophageal atresia and tracheoesophageal fistula. Pediatr Pulmonol. 2016;51:576–81. https://doi.org/10.1002/ppul.23330.
Fayoux P, Morisse M, Sfeir R, Michaud L, Daniel S. Laryngotracheal anomalies associated with esophageal atresia: importance of early diagnosis. Eur Archiv Otorhinolaryngol. 2018;275:477–81. https://doi.org/10.1007/s00405-017-4856-5.
Hysinger EB, Panitch HB. Paediatric tracheomalacia. Paediatr Respir Rev. 2016;17:9–15. https://doi.org/10.1016/j.prrv.2015.03.002.
Fraga JC, Jennings RW, Kim PC. Pediatric tracheomalacia. Semin Pediatr Surg. 2016;25:156–64. https://doi.org/10.1053/j.sempedsurg.2016.02.008.
Overman AE, Liu M, Kurachek SC, Shreve MR, Maynard RC, Mammel MC, Moore BM. Tracheostomy for infants requiring prolonged mechanical ventilation: 10 years’ experience. Pediatrics. 2013;131:e1491-1496. https://doi.org/10.1542/peds.2012-1943.
Wallis C, Alexopoulou E, Anton-Pacheco JL, Bhatt JM, Bush A, Chang AB, Charatsi AM, Coleman C, Depiazzi J, Douros K, Eber E, Everard M, Kantar A, Masters IB, Midulla F, Nenna R, Roebuck D, Snijders D, Priftis K. ERS statement on tracheomalacia and bronchomalacia in children. Eur Respir J. 2019. https://doi.org/10.1183/13993003.00382-2019.
Lee EY, Boiselle PM. Tracheobronchomalacia in infants and children: multidetector CT evaluation. Radiology. 2009;252:7–22. https://doi.org/10.1148/radiol.2513081280.
Fawcett SL, Gomez AC, Hughes JA, Set P. Anatomical variation in the position of the brachiocephalic trunk (innominate artery) with respect to the trachea: a computed tomography-based study and literature review of innominate artery compression syndrome. Clin Anat (New York, NY). 2010;23:61–9. https://doi.org/10.1002/ca.20884.
Ngerncham M, Lee EY, Zurakowski D, Tracy DA, Jennings R. Tracheobronchomalacia in pediatric patients with esophageal atresia: comparison of diagnostic laryngoscopy/bronchoscopy and dynamic airway multidetector computed tomography. J Pediatr Surg. 2015;50:402–7. https://doi.org/10.1016/j.jpedsurg.2014.08.021.
Lee EY, Mason KP, Zurakowski D, Waltz DA, Ralph A, Riaz F, Boiselle PM. MDCT assessment of tracheomalacia in symptomatic infants with mediastinal aortic vascular anomalies: preliminary technical experience. Pediatr Radiol. 2008;38:82–8. https://doi.org/10.1007/s00247-007-0672-1.
Sumida W, Tainaka T, Shirota C, Yokota K, Makita S, Takimoto A, Yasui A, Okamoto M, Nakagawa Y, Hinoki A, Uchida H. An imaging study on tracheomalacia in infants with esophageal atresia: the degree of tracheal compression by the brachiocephalic artery is a good indicator for therapeutic intervention. Pediatr Surg Int. 2021;37:1719–24. https://doi.org/10.1007/s00383-021-04985-0.
Sanchez MO, Greer MC, Masters IB, Chang AB. A comparison of fluoroscopic airway screening with flexible bronchoscopy for diagnosing tracheomalacia. Pediatr Pulmonol. 2012;47:63–7. https://doi.org/10.1002/ppul.21517.
Snijders D, Barbato A. An update on diagnosis of tracheomalacia in children. Eur J pediatr Surg. 2015;25:333–5. https://doi.org/10.1055/s-0035-1559816.
Masui D, Fukahori S, Hashizume N, Ishii S, Yagi M. High-flow nasal cannula therapy for severe tracheomalacia associated with esophageal atresia. Pediatr Int. 2019;61:1060–1. https://doi.org/10.1111/ped.13953.
Watters KF. Tracheostomy in infants and children. Respir Care. 2017;62:799–825. https://doi.org/10.4187/respcare.05366.
Gross RE. Neuhauser EB (1948) Compression of the trachea by an anomalous innominate artery; an operation for its relief. Am J Dis Child. 1911;75:570–4. https://doi.org/10.1001/archpedi.1948.02030020585007.
van der Zee DC, Straver M. Thoracoscopic aortopexy for tracheomalacia. World J Surg. 2015;39:158–64. https://doi.org/10.1007/s00268-014-2798-2.
Torre M, Carlucci M, Speggiorin S, Elliott MJ. Aortopexy for the treatment of tracheomalacia in children: review of the literature. Ital J Pediatr. 2012;38:62. https://doi.org/10.1186/1824-7288-38-62.
Williams SP, Losty PD, Dhannapuneni R, Lotto A, Guerrero R, Donne AJ. Aortopexy for the management of paediatric tracheomalacia—the Alder Hey experience. J Laryngol Otol. 2020. https://doi.org/10.1017/s0022215120000031.
Wong ZH, Hewitt R, Cross K, Butler C, Yeh YT, Ramaswamy M, Blackburn S, Giuliani S, Muthialu N, De Coppi P. Thoracoscopic aortopexy for symptomatic tracheobronchomalacia. J Pediatr Surg. 2020;55:229–33. https://doi.org/10.1016/j.jpedsurg.2019.10.034.
Haveliwala Z, Yardley I. Aortopexy for tracheomalacia via a suprasternal incision. J Pediatr Surg. 2019;54:247–50. https://doi.org/10.1016/j.jpedsurg.2018.10.073.
Rijnberg FM, Butler CR, Bieli C, Kumar S, Nouraei R, Asto J, McKavanagh E, de Coppi P, Muthialu N, Elliott MJ, Hewitt RJ. Aortopexy for the treatment of tracheobronchomalacia in 100 children: a 10-year single-centre experience. Eur J Cardio Thorac Surg. 2018;54:585–92. https://doi.org/10.1093/ejcts/ezy076.
Gruszka A, Sachweh JS, Schnoering H, Tenbrock K, Muehler EG, Laschat M, Vazquez-Jimenez JF. Aortopexy offers surgical options for a variety of pathological tracheal conditions in paediatric patients. Interact Cardiovasc Thorac Surg. 2017;25:589–94. https://doi.org/10.1093/icvts/ivx163.
Kay-Rivest E, Baird R, Laberge JM, Puligandla PS. Evaluation of aortopexy in the management of severe tracheomalacia after esophageal atresia repair. Dis Esophagus. 2015;28:234–9. https://doi.org/10.1111/dote.12179.
Jennings RW, Hamilton TE, Smithers CJ, Ngerncham M, Feins N, Foker JE. Surgical approaches to aortopexy for severe tracheomalacia. J Pediatr Surg. 2014;49:66–70. https://doi.org/10.1016/j.jpedsurg.2013.09.036. (discussion 70-61).
Arnaud AP, Rex D, Elliott MJ, Curry J, Kiely E, Pierro A, Cross K, De Coppi P. Early experience of thoracoscopic aortopexy for severe tracheomalacia in infants after esophageal atresia and tracheo-esophageal fistula repair. J Laparoendosc Adv Surg Tech A. 2014;24:508–12. https://doi.org/10.1089/lap.2013.0376.
Montgomery J, Sau C, Clement W, Danton M, Davis C, Haddock G, McLean A, Kubba H. Treatment of tracheomalacia with aortopexy in children in Glasgow. Eur J Pediatr Surg. 2014;24:389–93. https://doi.org/10.1055/s-0033-1351662.
Bairdain S, Zurakowski D, Baird CW, Jennings RW. Surgical treatment of tracheobronchomalacia: a novel approach. Paediatr Respir Rev. 2016;19:16–20. https://doi.org/10.1016/j.prrv.2016.04.002.
Shieh HF, Smithers CJ, Hamilton TE, Zurakowski D, Rhein LM, Manfredi MA, Baird CW, Jennings RW. Posterior tracheopexy for severe tracheomalacia. J Pediatr Surg. 2017;52:951–5. https://doi.org/10.1016/j.jpedsurg.2017.03.018.
van Tuyll van Serooskerken ES, Tytgat S, Verweij JW, Bittermann AJN, Coenraad S, Arets HGM, van der Zee DC, Lindeboom MYA. Primary posterior tracheopexy in esophageal atresia decreases respiratory tract infections. Front Pediatr. 2021;9:720618. https://doi.org/10.3389/fped.2021.720618.
Dewberry L, Wine T, Prager J, Masaracchia M, Janosy N, Polaner D, DeBoer E, Somme S. Thoracoscopic posterior tracheopexy is a feasible and effective treatment for tracheomalacia. J Laparoendosc Adv Surg Tech A. 2019;29:1228–31. https://doi.org/10.1089/lap.2019.0156.
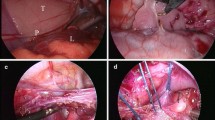
Tytgat S, van Herwaarden-Lindeboom MYA, van Tuyll van Serooskerken ES, van der Zee DC. Thoracoscopic posterior tracheopexy during primary esophageal atresia repair: a new approach to prevent tracheomalacia complications. J Pediatr Surg. 2018;53:1420–3. https://doi.org/10.1016/j.jpedsurg.2018.04.024.
Shieh HF, Smithers CJ, Hamilton TE, Zurakowski D, Visner GA, Manfredi MA, Baird CW, Jennings RW. Posterior tracheopexy for severe tracheomalacia associated with Esophageal Atresia (EA): primary treatment at the time of initial EA repair versus secondary treatment. Front Surg. 2017;4:80. https://doi.org/10.3389/fsurg.2017.00080.
Yasui A, Hinoki A, Amano H, Shirota C, Tainaka T, Sumida W, Yokota K, Makita S, Okamoto M, Takimoto A, Nakagawa Y, Uchida H. Thoracoscopic posterior tracheopexy during primary esophageal atresia repair ameliorate tracheomalacia in neonates: a single-center retrospective comparative cohort study. BMC Surg. 2022. https://doi.org/10.1186/s12893-022-01738-1.
Takazawa S, Uchida H, Kawashima H, Tanaka Y, Masuko T, Deie K, Nagase Y, Iwanaka T. External stabilization for severe tracheobronchomalacia using separated ring-reinforced ePTFE grafts is effective and safe on a long-term basis. Pediatr Surg Int. 2013;29:1165–9. https://doi.org/10.1007/s00383-013-3383-8.
Kamran A, Jennings RW. Tracheomalacia and tracheobronchomalacia in pediatrics: an overview of evaluation, medical management, and surgical treatment. Front Pediatr. 2019;7:512. https://doi.org/10.3389/fped.2019.00512.
Emery JL, Haddadin AJ. Squamous epithelium in respiratory tract of children with tracheo-oesophageal fistula. Arch Dis Child. 1971;46:236–42. https://doi.org/10.1136/adc.46.247.236.
Davies MR, Cywes S. The flaccid trachea and tracheoesophageal congenital anomalies. J Pediatr Surg. 1978;13:363–7. https://doi.org/10.1016/s0022-3468(78)80455-2.
Wailoo MP, Emery JL. Normal growth and development of the trachea. Thorax. 1982;37:584–7. https://doi.org/10.1136/thx.37.8.584.
Choi S, Lawlor C, Rahbar R, Jennings R. Diagnosis, classification, and management of pediatric tracheobronchomalacia: a review. JAMA Otolaryngol Head Neck Surg. 2019;145:265–75. https://doi.org/10.1001/jamaoto.2018.3276.
Gardella C, Girosi D, Rossi GA, Silvestri M, Toma P, Bava G, Sacco O. Tracheal compression by aberrant innominate artery: clinical presentations in infants and children, indications for surgical correction by aortopexy, and short- and long-term outcome. J Pediatr Surg. 2010;45:564–73. https://doi.org/10.1016/j.jpedsurg.2009.04.028.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sumida, W., Yasui, A., Shirota, C. et al. Update on aortopexy and posterior tracheopexy for tracheomalacia in patients with esophageal atresia. Surg Today 54, 211–219 (2024). https://doi.org/10.1007/s00595-023-02652-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02652-6