Abstract
Purpose
Early recurrence (ER) of rectal mucinous adenocarcinoma (MAC) has yet to be defined. We therefore explored risk factors for ER and constructed a predictive nomogram.
Method
A total of 145 rectal MAC patients undergoing radical surgery were included. The minimum P value method was used to determine the optimal cut-off point to discriminate between ER and late recurrence (LR). Risk factors for ER were determined by a logistic regression analysis, and a predictive nomogram was constructed.
Results
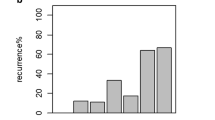
A total of 62 (42.8%) patients developed tumor recurrence. The optimal time to define ER was 12 months. A pre-treatment tumor distance from the anal verge ≤ 7 cm, pathological N stage, lymphovascular invasion, tumor deposits, and time to recurrence ≤ 12 months were significantly associated with a poor post-recurrence survival in patients with recurrence. A pre-treatment serum carcinoembryonic antigen (CEA) level > 10 ng/ml, pre-treatment tumor distance from the anal verge ≤ 7 cm, pathological N + stage, perineural invasion, and tumor deposits were identified as independent risk factors associated with ER. A nomogram predicting ER was constructed (C-index 0.870).
Conclusion
The pre-treatment serum CEA level, pre-treatment tumor distance from the anal verge, pathological N + stage, perineural invasion, and tumor deposits were significantly predictive of ER for rectal MAC patients.



Similar content being viewed by others
Data availability
Data not available due to ethical/legal restrictions.
References
Hyngstrom JR, Hu CY, Xing Y, You YN, Feig BW, Skibber JM, et al. Clinicopathology and outcomes for mucinous and signet ring colorectal adenocarcinoma: analysis from the national cancer data base. Ann Surg Oncol. 2012;19(9):2814–21.
Lan YT, Chang SC, Lin PC, Lin CC, Lin HH, Huang SC, et al. Clinicopathological and molecular features of colorectal cancer patients with mucinous and non-mucinous adenocarcinoma. Front Oncol. 2021;11: 620146.
Hugen N, Brown G, Glynne-Jones R, de Wilt JH, Nagtegaal ID. Advances in the care of patients with mucinous colorectal cancer. Nat Rev Clin Oncol. 2016;13(6):361–9.
Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012;30(16):1926–33.
van Gijn W, Marijnen CA, Nagtegaal ID, Kranenbarg EM, Putter H, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol. 2011;12(6):575–82.
Sun Y, Lin H, Lu X, Huang Y, Xu Z, Huang S, et al. A nomogram to predict distant metastasis after neoadjuvant chemoradiotherapy and radical surgery in patients with locally advanced rectal cancer. J Surg Oncol. 2017;115(4):462–9.
Guraya SY. Pattern, stage, and time of recurrent colorectal cancer after curative surgery. Clin Colorectal Cancer. 2019;18(2):e223–8.
Emile SH, Magdy A, Elnahas W, Hamdy O, Abdelnaby M, Khafagy W (2018) Predictors for local recurrence and distant metastasis of mucinous colorectal adenocarcinoma. Surgery
Furuke H, Arita T, Kuriu Y, Shimizu H, Kiuchi J, Yamamoto Y, et al. The survival after recurrence of colorectal cancer: a retrospective study focused on time to recurrence after curative resection. Surg Today. 2022;52(2):239–50.
Cho YB, Chun HK, Yun HR, Lee WS, Yun SH, Lee WY. Clinical and pathologic evaluation of patients with recurrence of colorectal cancer five or more years after curative resection. Dis Colon Rectum. 2007;50(8):1204–10.
Narayanan S, AlMasri S, Zenati M, Nassour I, Chopra A, Rieser C, et al. Predictors of early recurrence following neoadjuvant chemotherapy and surgical resection for localized pancreatic adenocarcinoma. J Surg Oncol. 2021;124(3):308–16.
Xing H, Sun LY, Yan WT, Quan B, Liang L, Li C, et al. Repeat hepatectomy for patients with early and late recurrence of hepatocellular carcinoma: a multicenter propensity score matching analysis. Surgery. 2021;169(4):911–20.
Park JS, Choe EA, Park S, Nam CM, Hyung WJ, Noh SH, et al. Detection of asymptomatic recurrence improves survival of gastric cancer patients. Cancer Med. 2021;10(10):3249–60.
Huh JW, Kim CH, Lim SW, Kim HR, Kim YJ. Early recurrence in patients undergoing curative surgery for colorectal cancer: is it a predictor for poor overall survival? Int J Colorectal Dis. 2013;28(8):1143–9.
Zheng Z, Wang X, Huang Y, Lu X, Huang Z, Chi P. Defining and predicting early recurrence in patients with locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Eur J Surg Oncol. 2020;46(11):2057–63.
Kim HG, Kim HS, Yang SY, Han YD, Cho MS, Hur H, et al. Early recurrence after neoadjuvant chemoradiation therapy for locally advanced rectal cancer: characteristics and risk factors. Asian J Surg. 2021;44(1):298–302.
Liu SL, Cheung WY. Role of surveillance imaging and endoscopy in colorectal cancer follow-up: quality over quantity? World J Gastroenterol. 2019;25(1):59–68.
Nga UK. Follow-up to detect recurrence after treatment for non-metastatic colorectal cancer: colorectal cancer (update): Evidence review E1. London: National Institute for Health and Care Excellence (NICE); 2020.
Lo DS, Pollett A, Siu LL, Gallinger S, Burkes RL. Prognostic significance of mesenteric tumor nodules in patients with stage III colorectal cancer. Cancer. 2008;112(1):50–4.
Nagtegaal ID, Knijn N, Hugen N, Marshall HC, Sugihara K, Tot T, et al. Tumor deposits in colorectal cancer: improving the value of modern staging-a systematic review and meta-analysis. J Clin Oncol. 2017;35(10):1119–27.
Lord AC, D’Souza N, Pucher PH, Moran BJ, Abulafi AM, Wotherspoon A, et al. Significance of extranodal tumour deposits in colorectal cancer: a systematic review and meta-analysis. Eur J Cancer. 2017;82:92–102.
Cohen R, Shi Q, Meyers J, Jin Z, Svrcek M, Fuchs C, et al. Combining tumor deposits with the number of lymph node metastases to improve the prognostic accuracy in stage III colon cancer: a post hoc analysis of the CALGB/SWOG 80702 phase III study (Alliance)(). Ann Oncol. 2021;32(10):1267–75.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al (2017) The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67(2):93–9
Edge SB, (2010) Compton CC The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–4
Groot VP, Gemenetzis G, Blair AB, Rivero-Soto RJ, Yu J, Javed AA, et al. Defining and predicting early recurrence in 957 patients with resected pancreatic ductal adenocarcinoma. Ann Surg. 2019;269(6):1154–62.
Hugen N, van de Velde C, de Wilt J, Nagtegaal ID. Metastatic pattern in colorectal cancer is strongly influenced by histological subtype. Ann Oncol. 2014;25(3):651–7.
Mitry E, Guiu B, Cosconea S, Jooste V, Faivre J, Bouvier AM. Epidemiology, management and prognosis of colorectal cancer with lung metastases: a 30-year population-based study. Gut. 2010;59(10):1383–8.
Nordholm-Carstensen A, Krarup PM, Jorgensen LN, Wille-Jorgensen PA, Harling H. Occurrence and survival of synchronous pulmonary metastases in colorectal cancer: a nationwide cohort study. Eur J Cancer. 2014;50(2):447–56.
Riihimaki M, Hemminki A, Sundquist J, Hemminki K. Patterns of metastasis in colon and rectal cancer. Sci Rep. 2016;6:29765.
Wu S, Gu W. Association of T Stage and Serum CEA Levels in determining survival of rectal cancer. Front Med (Lausanne). 2019;6:270.
Pu H, Xie P, Chen Y, Zhao Y, Ye X, Lu G, et al. Relationship between preoperative and postoperative serum carcinoembryonic antigen and prognosis of patients with stage I-III rectal cancer: a retrospective study of a multicentre cohort of 1022 rectal cancer patients. Cancer Manag Res. 2021;13:2643–51.
Yang H, Yao Z, Cui M, Xing J, Zhang C, Zhang N, et al. Influence of tumor location on short- and long-term outcomes after laparoscopic surgery for rectal cancer: a propensity score matched cohort study. BMC Cancer. 2020;20(1):761.
Augestad KM, Keller DS, Bakaki PM, Rose J, Koroukian SM, Oresland T, et al. The impact of rectal cancer tumor height on recurrence rates and metastatic location: a competing risk analysis of a national database. Cancer Epidemiol. 2018;53:56–64.
Leibold T, Shia J, Ruo L, Minsky BD, Akhurst T, Gollub MJ, et al. Prognostic implications of the distribution of lymph node metastases in rectal cancer after neoadjuvant chemoradiotherapy. J Clin Oncol. 2008;26(13):2106–11.
Kim CH, Yeom SS, Lee SY, Kim HR, Kim YJ, Lee KH, et al. Prognostic impact of perineural invasion in rectal cancer after neoadjuvant chemoradiotherapy. World J Surg. 2019;43(1):260–72.
Delattre JF, Cohen R, Henriques J, Falcoz A, Emile JF, Fratte S, et al. Prognostic value of tumor deposits for disease-free survival in patients with stage iii colon cancer: a post hoc analysis of the IDEA france phase III trial (PRODIGE-GERCOR). J Clin Oncol. 2020;38(15):1702–10.
Alnimer Y, Ghamrawi R, Aburahma A, Salah S, Rios-Bedoya C, Katato K. Factors associated with short recurrence-free survival in completely resected colon cancer. J Community Hosp Intern Med Perspect. 2017;7(6):341–6.
Primrose JN, Perera R, Gray A, Rose P, Fuller A, Corkhill A, et al. Effect of 3–5 years of scheduled CEA and CT follow-up to detect recurrence of colorectal cancer: the FACS randomized clinical trial. JAMA. 2014;311(3):263–70.
Steele SR, Chang GJ, Hendren S, Weiser M, Irani J, Buie WD, et al. Practice guideline for the surveillance of patients after curative treatment of colon and rectal cancer. Dis Colon Rectum. 2015;58(8):713–25.
Kennedy E, Zwaal C, Asmis T, Cho C, Galica J, Ginty A, et al. An evidence-based guideline for surveillance of patients after curative treatment for colon and rectal cancer. Curr Oncol. 2022;29(2):724–40.
Acknowledgements
The authors thank all the staff in the Department of colorectal surgery, Fujian Medical University Union Hospital, Fuzhou, Fujian Province, PR China.
Funding
This study was supported by the Construction Project of Fujian Province Minimally Invasive Medical Center ([2017]171), Joint Funds for the Innovation of Science and Technology, Fujian province (2018Y9030, 2019Y9101, 2019Y9061), Young and Middle-aged Backbone Training Project in the Health System of Fujian province (2019-ZQN-45), Natural Science Foundation of Fujian Province (2020J011030), and Medical Science Research Foundation of Beijing Medical and Health Foundation (B20062DS), Fujian provincial health technology project (2020CXA025), and Bethune Charitable Foundation (X-J-2018–004).
Author information
Authors and Affiliations
Contributions
Yanwu Sun, Yu Deng, and Pan Chi designed the study. Yanwu Sun, Yu Deng, Meifang Xu, and Jingming Zhong collected the data and were major contributors to writing the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, Y., Deng, Y., Xu, M. et al. A refined prediction of early recurrence combining tumor deposits in patients with resected rectal mucinous adenocarcinoma. Surg Today 53, 762–772 (2023). https://doi.org/10.1007/s00595-022-02613-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02613-5