Abstract
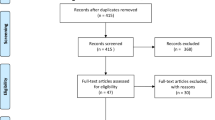
The supraclavicular lymph nodes (SCLNs) have been regarded as regional nodes for esophageal squamous cell carcinoma (ESCC) in Japan and eastern Asian countries, whereas their involvement has been regarded as distant metastasis in Western countries. The importance of thorough dissection of the lymphatic chain along the recurrent laryngeal nerve, including the cervical paraesophageal nodes, has become well understood; therefore, the contemporary clinical question is whether prophylactic SCLN dissection (SLND) in addition to cervical paraesophageal node dissection is beneficial for patients with ESCC. We analyzed studies comparing esophagectomy with SLND vs. esophagectomy without SLND, in both of which cervical paraesophageal node dissection had been completed, based on a comprehensive literature search of the PubMed, Scopus, and Cochrane databases. Our meta-analysis focused on two long-term outcomes: 3-year and 5-year overall survival (OS) rates; and three short-term outcomes: pneumonia, recurrent nerve palsy, and anastomotic leakage. Four studies, with a collective total of 1584 patients were included in the review. No significant differences were found between esophagectomy with SLND vs. esophagectomy without SLND in the meta-analysis of both long-term (3-year and 5-year OS; risk ratio 1.09, 95% CI 0.94–1.26, P = 0.28, and risk ratio 1.14, 95% CI 0.96–1.35, P = 0.15, respectively) and short-term outcomes. Based on our analysis, no clear data support prophylactic SLND on the cervical paraesophageal node dissection.







Similar content being viewed by others
References
Kitagawa Y, Uno T, Oyama T, Kato K, Kato H, Kawakubo H, et al. Esophageal cancer practice guidelines 2017 edited by the Japan esophageal society: part 1. Esophagus. 2019;16:1–24.
Kitagawa Y, Uno T, Oyama T, Kato K, Kato H, Kawakubo H, et al. Esophageal cancer practice guidelines 2017 edited by the Japan esophageal society: part 2. Esophagus. 2019;16:25–43.
Lordick F, Mariette C, Haustermans K, Obermannová R, Arnold D, EG Committee. Oesophageal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27:v50–7.
Ajani JA, D’Amico TA, Bentrem DJ, Chao J, Corvera C, Das P, et al. Esophageal and esophagogastric junction cancers, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(855):883.
Japan Esophageal Society. Japanese classification of esophageal cancer, 11th edition: part I. Esophagus. 2017;14:1–36.
Brierley JD, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours, 8th Edition. Wiley-Blackwell, 2016.
Akiyama H, Tsurumaru M, Udagawa H, Kajiyama Y. Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg. 1994;220:364–72.
Ando N, Ozawa S, Kitagawa Y, Shinozawa Y, Kitajima M. Improvement in the results of surgical treatment of advanced squamous esophageal carcinoma during 15 consecutive years. Ann Surg. 2000;232:225–32.
Isono K, Ochiai T, Okuyama K, Onoda S. The treatment of lymph node metastasis from esophageal cancer by extensive lymphadenectomy. Jpn J Surg. 1990;20:151–7.
Tsunoda S, Shinohara H, Kanaya S, Okabe H, Tanaka E, Obama K, et al. Mesenteric excision of upper esophagus: a concept for rational anatomical lymphadenectomy of the recurrent laryngeal nodes in thoracoscopic esophagectomy. Surg Endosc. 2020;34:133–41.
Tachimori Y, Ozawa S, Numasaki H, Matsubara H, Shinoda M, Toh Y, et al. Supraclavicular node metastasis from thoracic esophageal carcinoma: a surgical series from a Japanese multi-institutional nationwide registry of esophageal cancer. J Thorac Cardiovasc Surg. 2014;148:1224–9.
Tachimori Y, Ozawa S, Numasaki H, Matsubara H, Shinoda M, Toh Y, et al. Efficacy of lymph node dissection for each station based on esophageal tumor location. Esophagus. 2016;13:138–45.
Udagawa H, Ueno M, Shinohara H, Haruta S, Kaida S, Nakagawa M, et al. The importance of grouping of lymph node stations and rationale of three-field lymphoadenectomy for thoracic esophageal cancer. J Surg Oncol. 2012;106:742–7.
Kato H. Lymph node dissection for thoracic esophageal carcinoma. Two- and 3-field lymph node dissection. Ann Chir Gynaecol. 1995;84:193–9.
Yamashita K, Makino T, Yamasaki M, Tanaka K, Hara T, Miyazaki Y, et al. Comparison of short-term outcomes between 2- and 3-field lymph node dissection for esophageal cancer. Dis Esophagus. 2017;30:1–8.
Mine S, Watanabe M, Kumagai K, Okamura A, Yamashita K, Hayami M, et al. Oesophagectomy with or without supraclavicular lymphadenectomy after neoadjuvant treatment for squamous cell carcinoma of the oesophagus. Br J Surg. 2018;105:1793–8.
Koterazawa Y, Oshikiri T, Takiguchi G, Hasegawa H, Yamamoto M, Kanaji S, et al. Prophylactic cervical lymph node dissection in thoracoscopic esophagectomy for esophageal cancer increases postoperative complications and does not improve survival. Ann Surg Oncol. 2019;26:2899–904.
Ma GW, Situ DR, Ma QL, Long H, Zhang LJ, Lin P, et al. Three-field vs two-field lymph node dissection for esophageal cancer: a meta-analysis. World J Gastroenterol. 2014;20:18022–30.
Ye T, Sun Y, Zhang Y, Zhang Y, Chen H. Three-field or two-field resection for thoracic esophageal cancer: a meta-analysis. Ann Thorac Surg. 2013;96:1933–41.
Wang J, Yang Y, Shafiulla Shaik M, Hu J, Wang K, Gao C, et al. Three-field versus two-field lymphadenectomy for esophageal squamous cell carcinoma: a meta-analysis. J Surg Res. 2020;255:195–204.
Bona D, Lombardo F, Matsushima K, Cavalli M, Lastraioli C, Bonitta G, et al. Three-field versus two-field lymphadenectomy for esophageal squamous cell carcinoma: a long-term survival meta-analysis. Surgery. 2021;171(4):940–7.
Law S, Wong J. Two-field dissection is enough for esophageal cancer. Dis Esophagus. 2001;14:98–103.
Li B, Hu H, Zhang Y, Zhang J, Miao L, Ma L, et al. Three-field versus two-field lymphadenectomy in transthoracic oesophagectomy for oesophageal squamous cell carcinoma: short-term outcomes of a randomized clinical trial. Br J Surg. 2020;107:647–54.
Li B, Zhang Y, Miao L, Ma L, Luo X, Zhang Y, et al. Esophagectomy with three-field versus two-field lymphadenectomy for middle and lower thoracic esophageal cancer: long-term outcomes of a randomized clinical trial. J Thorac Oncol. 2021;16:310–7.
Yano M, Takachi K, Doki Y, Miyashiro I, Kishi K, Noura S, et al. Prognosis of patients who develop cervical lymph node recurrence following curative resection for thoracic esophageal cancer. Dis Esophagus. 2006;19:73–7.
Ma X, Zhao K, Guo W, Yang S, Zhu X, Xiang J, et al. Salvage lymphadenectomy versus salvage radiotherapy/chemoradiotherapy for recurrence in cervical lymph node after curative resection of esophageal squamous cell carcinoma. Ann Surg Oncol. 2015;22:624–9.
Kato K, Ito Y, Nozaki I, Daiko H, Kojima T, Yano M, et al. Parallel-group controlled trial of surgery versus chemoradiotherapy in patients with stage I esophageal squamous cell carcinoma. Gastroenterology. 2021;161:1878-1886.e1872.
Nishihira T, Hirayama K, Mori S. A prospective randomized trial of extended cervical and superior mediastinal lymphadenectomy for carcinoma of the thoracic esophagus. Am J Surg. 1998;175:47–51.
Funding
None.
Author information
Authors and Affiliations
Contributions
ST and NH contributed to the study concept and design. Literature search and data collection were performed by NH and SY. Statistical analysis was conducted by NH and SY and then checked by the other authors. The first draft of the manuscript was written by ST, and all authors commented on the previous version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare in relation to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix S1
Search strategy for pubmed
#1 "Esophageal Neoplasms"[MeSH Terms].
#2 esophagus[Tiab] OR esophageal[Tiab] OR oesophagus[Tiab] OR oesophageal[Tiab].
#3 neoplasm[Tiab] OR cancer[Tiab] OR tumor[Tiab] OR carcinoma[Tiab].
#4 #2 AND #3
#5 #1 OR #4
#6 three-field[Tiab] OR 3-field[Tiab] OR supraclavicular[Tiab] OR cervical[Tiab] OR neck[Tiab] OR extensive[Tiab] OR extended[Tiab].
#7 "Lymph Node Excision"[MeSH Terms].
#8 dissection[Tiab] OR lymphadenectomy[Tiab].
#9 #7 OR #8
#10 #6 AND #9
#11 #5 AND #10
#12 #11 AND english[la].
Rights and permissions
About this article
Cite this article
Tsunoda, S., Hoshino, N., Yoshida, S. et al. Prophylactic supraclavicular lymph node dissection for esophageal squamous cell carcinoma: a systematic review and meta-analysis. Surg Today 53, 647–654 (2023). https://doi.org/10.1007/s00595-022-02544-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02544-1