Abstract
Purpose
Anaplastic thyroid cancer (ATC) is a highly aggressive tumor that invades surrounding tissues and rapidly metastasizes throughout the body. Growth of the primary tumor in the neck often causes serious conditions that decrease the quality of life (QOL) of patients. The objective of this study was to investigate the role of surgical resection in improving the QOL of patients with ATC.
Methods
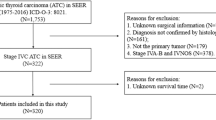
This was a retrospective review of 62 patients with ATC treated at Shinshu University Hospital between January 2001 and June 2019.
Results
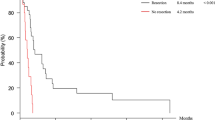
Fourteen patients underwent R0/R1 resection. Thirteen of the 14 patients received postoperative radiation, and 4 received chemotherapy. The mean survival period was 15.4 ± 18.2 (range, 2–75) months. Distant metastases appeared within 3.2 ± 2.3 months postoperatively in 12 patients. A permanent tracheostomy was required in six patients; however, eight patients did not show airway obstruction until death. Daily treatment for exudate or bleeding from tumors that eroded in the neck, which deteriorated the QOL, was unnecessary in 12 patients.
Conclusions
As surgical resection can improve the QOL in patients with ATC, thyroid surgeons should promptly and carefully evaluate the resectability of the tumor and favor resection as much as possible.

Similar content being viewed by others
Data availability
Please contact the author for data requests.
References
Prasongsook N, Kumar A, Chintakuntlawar AV, Foote RL, Kasperbauer J, Molina J, et al. Survival in response to multimodal therapy in anaplastic thyroid cancer. J Clin Endocrinol Metab. 2017;102:4506–14.
Lin B, Ma H, Ma M, Zhang Z, Sun Z, Hsieh IY, et al. The incidence and survival analysis for anaplastic thyroid cancer: a SEER database analysis. Am J Transl Res. 2019;11:5888–96.
Are C, Shaha AR. Anaplastic thyroid carcinoma: biology, pathogenesis, prognostic factors, and treatment approaches. Ann Surg Oncol. 2006;13:453–64.
Smallridge RC, Marlow LA, Copland JA. Anaplastic thyroid cancer: molecular pathogenesis and emerging therapies. Endocr Relat Cancer. 2009;16:17–44.
Sugitani I, Onoda N, Ito KI, Suzuki S. Management of anaplastic thyroid carcinoma: the fruits from the ATC Research Consortium of Japan. J Nippon Med Sch. 2018;85:18–27.
Smallridge RC, Ain KB, Asa SL, Bible KC, Brierley JD, Burman KD, et al. American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2012;22:1104–39.
Rao SN, Zafereo M, Dadu R, Busaidy NL, Hess K, Cote GJ, et al. Patterns of treatment failure in anaplastic thyroid carcinoma. Thyroid. 2017;27:672–81.
Moyer KF, Marcadis AR, Shaha AR. Airway management, symptom relief and best supportive care in anaplastic thyroid cancer. Curr Opin Otolaryngol Head Neck Surg. 2020;28:74–8.
Ito K, Hanamura T, Murayama K, Okada T, Watanabe T, Harada M, et al. Multimodality therapeutic outcomes in anaplastic thyroid carcinoma: improved survival in subgroups of patients with localized primary tumors. Head Neck. 2012;34:230–7.
Bisof V, Rakusic Z, Despot M. Treatment of patients with anaplastic thyroid cancer during the last 20 years: whether any progress has been made? Eur Arch Otorhinolaryngol. 2015;272:1553–67.
Maniakas A, Dadu R, Busaidy NL, Wang JR, Ferrarotto R, Lu C, et al. Evaluation of overall survival in patients with anaplastic thyroid carcinoma, 2000–2019. JAMA Oncol. 2020;6:1397–404.
Mani N, McNamara K, Lowe N, Loughran S, Yap BK. Management of the compromised airway and role of tracheotomy in anaplastic thyroid carcinoma. Head Neck. 2016;38:85–8.
Bible KC, Kebebew E, Brierley J, Brito JP, Cabanillas ME, Clark TJ Jr, et al. 2021 American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2021;31:337–86.
Chiacchio S, Lorenzoni A, Boni G, Rubello D, Elisei R, Mariani G. Anaplastic thyroid cancer: prevalence, diagnosis and treatment. Minerva Endocrinol. 2008;33:341–57.
Lowe NM, Loughran S, Slevin NJ, Yap BK. Anaplastic thyroid cancer: the addition of systemic chemotherapy to radiotherapy led to an observed improvement in survival—a single centre experience and review of the literature. ScientificWorldJournal. 2014;2014: 674583.
Sugino K, Ito K, Mimura T, Nagahama M, Fukunari N, Kubo A, et al. The important role of operations in the management of anaplastic thyroid carcinoma. Surgery. 2002;131:245–8.
Mohebati A, Dilorenzo M, Palmer F, Patel SG, Pfister D, Lee N, et al. Anaplastic thyroid carcinoma: a 25-year single-institution experience. Ann Surg Oncol. 2014;21:1665–70.
Nachalon Y, Stern-Shavit S, Bachar G, Shvero J, Limon D, Popovtzer A. Aggressive palliation and survival in anaplastic thyroid carcinoma. JAMA Otolaryngol Head Neck Surg. 2015;141:1128–32.
Baek SK, Lee MC, Hah JH, Ahn SH, Son YI, Rho YS, et al. Role of surgery in the management of anaplastic thyroid carcinoma: Korean nationwide multicenter study of 329 patients with anaplastic thyroid carcinoma, 2000 to 2012. Head Neck. 2017;39:133–9.
Subbiah V, Kreitman RJ, Wainberg ZA, Cho JY, Schellens JHM, Soria JC, et al. Dabrafenib and trametinib treatment in patients with locally advanced or metastatic BRAF V600-mutant anaplastic thyroid cancer. J Clin Oncol. 2018;36:7–13.
Doebele RC, Drilon A, Paz-Ares L, Siena S, Shaw AT, Farago AF, et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours: integrated analysis of three phase 1–2 trials. Lancet Oncol. 2020;21:271–82.
Wirth LJ, Sherman E, Robinson B, Solomon B, Kang H, Lorch J, et al. Efficacy of selpercatinib in RET-altered thyroid cancers. N Engl J Med. 2020;383:825–35.
NCC Network. NCCN Clinical Practice Guidelines in Oncology, Thyroid Carcinoma 2021;Version 1.2021.
Cabanillas ME, Ryder M, Jimenez C. Targeted therapy for advanced thyroid cancer: kinase inhibitors and beyond. Endocr Rev. 2019;40:1573–604.
Cabanillas ME, Ferrarotto R, Garden AS, Ahmed S, Busaidy NL, Dadu R, et al. Neoadjuvant BRAF- and immune-directed therapy for anaplastic thyroid carcinoma. Thyroid. 2018;28:945–51.
Wang JR, Zafereo ME, Dadu R, Ferrarotto R, Busaidy NL, Lu C, et al. Complete surgical resection following neoadjuvant dabrafenib plus trametinib in BRAF(V600E)-mutated anaplastic thyroid carcinoma. Thyroid. 2019;29:1036–43.
Ricarte-Filho JC, Ryder M, Chitale DA, Rivera M, Heguy A, Ladanyi M, et al. Mutational profile of advanced primary and metastatic radioactive iodine-refractory thyroid cancers reveals distinct pathogenetic roles for BRAF, PIK3CA, and AKT1. Cancer Res. 2009;69:4885–93.
Nikiforova MN, Kimura ET, Gandhi M, Biddinger PW, Knauf JA, Basolo F, et al. BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab. 2003;88:5399–404.
Takano T, Ito Y, Hirokawa M, Yoshida H, Miyauchi A. BRAF V600E mutation in anaplastic thyroid carcinomas and their accompanying differentiated carcinomas. Br J Cancer. 2007;96:1549–53.
Landa I, Ibrahimpasic T, Boucai L, Sinha R, Knauf JA, Shah RH, et al. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J Clin Investig. 2016;126:1052–66.
Bonhomme B, Godbert Y, Perot G, Al Ghuzlan A, Bardet S, Belleannee G, et al. Molecular pathology of anaplastic thyroid carcinomas: a retrospective study of 144 cases. Thyroid. 2017;27:682–92.
Cabanillas ME, Williams MD, Gunn GB, Weitzman SP, Burke L, Busaidy NL, et al. Facilitating anaplastic thyroid cancer specialized treatment: a model for improving access to multidisciplinary care for patients with anaplastic thyroid cancer. Head Neck. 2017;39:1291–5.
Acknowledgements
We would like to thank Editage (http://www.editage.jp) for the English language editing.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
All of the authors were involved in the management of the patients. TK and KI contributed to the drafting and the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Institutional review board statement
This study was approved by the Institutional Review Board of Shinshu University School of Medicine (No. 4920).
Informed consent
Written informed consent was obtained from the patients regarding the use of their clinical information.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kanai, T., Ito, T., Morikawa, H. et al. Surgical resection of the primary tumor prevents an undesirable locoregional condition and improves the quality of life in patients with anaplastic thyroid cancer. Surg Today 52, 1620–1626 (2022). https://doi.org/10.1007/s00595-022-02494-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02494-8