Abstract
Purpose
A circumferential resection margin (CRM) > 1 mm is a surrogate marker of oncologic outcomes in rectal cancer patients. In Japan, because the mesentery is removed from the rectum, the CRM cannot be measured. This multicenter prospective study evaluates the feasibility of a resected specimen processing method that allows CRM measurement.
Methods
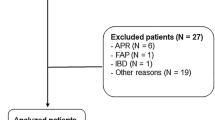
Fifty patients with rectal cancer were enrolled. Resected specimens were processed as previously reported. The primary outcomes were CRM measurement and the rate of CRM positivity. The secondary outcomes were the quality of total mesorectal excision, the possibility to visualize and sample the tumor, the number of harvested lymph nodes, and comparison between the pathological CRM and preoperative mesorectal fascia (MRF) involvement. This study was registered in the University Hospital Medical Information Network (UMIN) Clinical Trials Registry under identification number UMIN000031735.
Results
The CRM was measurable in all patients and found to be positive in three (6%). We confirmed tumor localization, sampled the tumor, and measured the distal margin in all patients. A median of 20 lymph nodes were harvested. The concordance rate between preoperative MRF involvement and pathological CRM status was 90%.
Conclusion
A semi-opened rectal specimen with transverse slicing is a feasible method for measuring the CRM.




Similar content being viewed by others
Data availability
The data produced and analyzed for this study are available from the corresponding author on reasonable request.
References
Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery–the clue to pelvic recurrence? Br J Surg. 1982;69:613–6.
Heald RJ, Moran BJ. Embryology and anatomy of the rectum. Semin Surg Oncol. 1998;15:66–71.
Glynne-Jones R, Wyrwicz L, Tiret E, Brown G, Rödel C, Cervantes A, et al. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv22–40.
Quirke P, Steele R, Monson J, Grieve R, Khanna S, Couture J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet. 2009;373:821–8.
Shirouzu K, Isomoto H, Kakegawa T. Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer. 1995;76:388–92.
Adam IJ, Mohamdee MO, Martin IG, Scott N, Finan PJ, Johnston D, et al. Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet. 1994;344:707–11.
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014;15:767–74.
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372:1324–32.
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, et al. Effect of laparoscopic-assisted resection vs open resection of Stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA. 2015;314:1346–55.
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA. 2015;314:1356–63.
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA. 2017;318:1569–80.
Roodbeen SX, de Lacy FB, van Dieren S, Penna M, Ris F, Moran B, et al. Predictive factors and risk model for positive circumferential resection margin rate after transanal total mesorectal excision in 2653 patients with rectal cancer. Ann Surg. 2019;270:884–91.
Taylor FG, Quirke P, Heald RJ, Moran BJ, Blomqvist L, Swift IR, et al. Preoperative magnetic resonance imaging assessment of circumferential resection margin predicts disease-free survival and local recurrence: 5-year follow-up results of the mercury study. J Clin Oncol. 2014;32:34–43.
Japanese society for cancer of the colon and rectum. Japanese classification of colorectal, appendiceal, and anal carcinoma: the 3d english edition [secondary publication]. J Anus Rectum Colon English. 2019;3:175–95.
Kurisu Y, Shimoda T, Ochiai A, Nakanishi Y, Hirata I, Katsu KI. Histologic and immunohistochemical analysis of early submucosal invasive carcinoma of the colon and rectum. Pathol Int. 1999;49:608–16.
Ishii M, Takemasa I, Okita K, Okuya K, Hamabe A, Nishidate T, et al. A modified method for resected specimen processing in rectal cancer: semi-opened with transverse slicing for measuring of the circumferential resection margin. Asian J Endosc Surg. 2021. https://doi.org/10.1111/ases.13003.
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, et al. Incidence and risk factors for anastomotic failure in 1594 patients treated by transanal total mesorectal excision: results from the international TaTME registry. Ann Surg. 2019;269:700–11.
Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH. Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol. 2002;26:350–7.
Hida K, Okamura R, Sakai Y, Konishi T, Akagi T, Yamaguchi T, et al. Open versus laparoscopic surgery for advanced low rectal cancer: a large, multicenter, propensity score matched cohort study in Japan. Ann Surg. 2018;268:318–24.
Patel A, Green N, Sarmah P, Langman G, Chandrakumaran K, Youssef H. The clinical significance of a pathologically positive lymph node at the circumferential resection margin in rectal cancer. Tech Coloproctol. 2019;23:151–9.
MERCURY study group. Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ. 2006;333:779.
Acknowledgements
We thank Drs M Kojima, T Yoshida, T Sakurai, H Kawachi, T Daa, and U Itai for their contribution as advisors on pathology, and Y Tsukada, T Nakamura, K Hida, and H Shiroshita for their contribution to the data collection.
Funding
No funding was received for the conduct of this research and or its publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. K Okuya, I Takemasa, K Okita, M Ishii, M Ito, K Uehara, S Yamaguchi, M Inomata, S Sugita, T Hasegawa, A Ochiai, Y Sakai, and M Watanabe have no conflicts of interest to declare. Dr T Konishi received honoraria from Johnson and Johnson Japan and Medtronic Japan.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Takemasa, I., Okuya, K., Okita, K. et al. Feasibility of the semi-opened method of specimen resection for a circumferential resection margin in rectal cancer surgery: a multicenter study. Surg Today 52, 1275–1283 (2022). https://doi.org/10.1007/s00595-022-02481-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02481-z