Abstract
Purpose
This retrospective study aimed to clarify whether the postoperative prognosis differs between right and left hepatectomy for Bismuth type I/II perihilar cholangiocarcinoma.
Methods
Preoperative images of 195 patients with perihilar cholangiocarcinoma were reexamined. Patients with Bismuth type I/II perihilar cholangiocarcinoma without a difference in extraductal tumor invasion between the right and left sides of the hepatic portal region were classified into those undergoing left (L group) or right (R group) hepatectomy.
Results
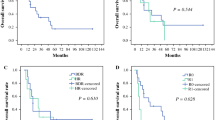
Twenty-three patients (11.8%) were classified into the L group and 33 (16.9%) into the R group. All eight patients with pTis/1 belonged to the L group. The L group had significantly less liver failure than the R group (p = 0.001). One patient (4.3%) in the L group and four patients (12.1%) in the R group died from postoperative complications. Among 48 patients with pT2, the L group tended to have better overall survival (median, 12.2 vs. 5.6 years; p = 0.072), but not recurrence-free survival (median, 9.1 vs. 3.6 years; p = 0.477), in comparison to the R group.
Conclusions
Postoperative survival after left hepatectomy for Bismuth type I/II perihilar cholangiocarcinoma is expected to be as long as that after right hepatectomy.



Similar content being viewed by others
Change history
18 November 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00595-021-02410-6
References
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. 8th ed. New York: Springer; 2016.
Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992;215:31–8.
Kawasaki S, Imamura H, Kobayashi A, Noike T, Miwa S, Miyagawa S. Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg. 2003;238:84–92.
Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004;240:95–101.
Ikeyama T, Nagino M, Oda K, Ebata T, Nishio H, Nimura Y. Surgical approach to bismuth Type I and II hilar cholangiocarcinomas: audit of 54 consecutive cases. Ann Surg. 2007;246:1052–7.
Neuhaus P, Thelen A, Jonas S, Puhl G, Denecke T, Veltzke-Schlieker W, et al. Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann Surg Oncol. 2012;19:1602–8.
Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K. No-touch resection of hilar malignancies with right hepatectomy and routine portal reconstruction. J Hepatobiliary Pancreat Surg. 2009;16:502–7.
Tamoto E, Hirano S, Tsuchikawa T, Tanaka E, Miyamoto M, Matsumoto J, et al. Portal vein resection using the no-touch technique with a hepatectomy for hilar cholangiocarcinoma. HPB (Oxford). 2014;16:56–61.
Nagino M, Ebata T, Mizuno T. Oncological superiority of right-sided hepatectomy over left-sided hepatectomy as surgery for klatskin tumors: truth or biased view? Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000004534.
Mueller M, Breuer E, Mizuno T, Bartsch F, Ratti F, Benzing C, et al. Perihilar cholangiocarcinoma-novel benchmark values for surgical and oncological outcomes from 24 expert centers. Ann Surg. 2021. https://doi.org/10.1097/SLA.0000000000005103.
Hirose T, Igami T, Ebata T, Yokoyama Y, Sugawara G, Mizuno T, et al. Surgical and radiological studies on the length of the hepatic ducts. World J Surg. 2015;39:2983–9.
Nakanishi Y, Tsuchikawa T, Okamura K, Nakamura T, Tamoto E, Noji T, et al. Risk factors for a high Comprehensive Complication Index score after major hepatectomy for biliary cancer: a study of 229 patients at a single institution. HPB (Oxford). 2016;18:735–41.
Hirano S, Tanaka E, Shichinohe T, Suzuki O, Hazama K, Kitagami H, et al. Treatment strategy for hilar cholangiocarcinoma, with special reference to the limits of ductal resection in right-sided hepatectomies. J Hepatobiliary Pancreat Surg. 2007;14:429–33.
Noji T, Tanaka K, Matsui A, Nakanishi Y, Asano T, Nakamura T, et al. Transhepatic direct approach to the “limit of the division of the hepatic ducts” leads to a high r0 resection rate in perihilar cholangiocarcinoma. J Gastrointest Surg. 2021;25:2358–67.
Sakuhara Y, Abo D, Hasegawa Y, Shimizu T, Kamiyama T, Hirano S, et al. Preoperative percutaneous transhepatic portal vein embolization with ethanol injection. AJR Am J Roentgenol. 2012;198:914–22.
Nakanishi Y, Tsuchikawa T, Okamura K, Nakamura T, Tamoto E, Murakami S, et al. Prognostic impact of the site of portal vein invasion in patients with surgically resected perihilar cholangiocarcinoma. Surgery. 2016;159:1511–9.
Uesaka K. Left hepatectomy or left trisectionectomy with resection of the caudate lobe and extrahepatic bile duct for hilar cholangiocarcinoma (with video). J Hepatobiliary Pancreat Sci. 2012;19:195–202.
Natsume S, Ebata T, Yokoyama Y, Igami T, Sugawara G, Shimoyama Y, et al. Clinical significance of left trisectionectomy for perihilar cholangiocarcinoma: an appraisal and comparison with left hepatectomy. Ann Surg. 2012;255:754–62.
Hirano S, Tanaka E, Tsuchikawa T, Matsumoto J, Shichinohe T, Kato K. Techniques of biliary reconstruction following bile duct resection (with video). J Hepatobiliary Pancreat Sci. 2012;19:203–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
Rahbari NN, Garden OJ, Padbury R, Maddern G, Koch M, Hugh TJ, et al. Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford). 2011;13:528–35.
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–8.
Nakanishi Y, Okamura K, Tsuchikawa T, Nakamura T, Noji T, Asano T, et al. Time to recurrence after surgical resection and survival after recurrence among patients with perihilar and distal cholangiocarcinomas. Ann Surg Oncol. 2020;27:4171–80.
Mizuno T, Ebata T, Yokoyama Y, Igami T, Yamaguchi J, Onoe S, et al. Combined vascular resection for locally advanced perihilar cholangiocarcinoma. Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000004322.
Matsuyama R, Mori R, Ota Y, Homma Y, Kumamoto T, Takeda K, et al. Significance of vascular resection and reconstruction in surgery for hilar cholangiocarcinoma: with special reference to hepatic arterial resection and reconstruction. Ann Surg Oncol. 2016;23:475–84.
Sugiura T, Okamura Y, Ito T, Yamamoto Y, Ashida R, Ohgi K, et al. Left hepatectomy with combined resection and reconstruction of right hepatic artery for bismuth type i and ii perihilar cholangiocarcinoma. World J Surg. 2019;43:894–901.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Reference 12 was published incorrectly in the original publication. Reference 12 has been updated in original publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nakanishi, Y., Hirano, S., Okamura, K. et al. Clinical and oncological benefits of left hepatectomy for Bismuth type I/II perihilar cholangiocarcinoma. Surg Today 52, 844–852 (2022). https://doi.org/10.1007/s00595-021-02401-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02401-7