Abstract
Purpose
We sometimes experienced prolonged delayed gastric emptying (DGE) in neurologically impaired patients undergoing laparoscopic fundoplication and gastrostomy. We explored the difference in the DGE rate according to the preoperative stomach position.
Methods
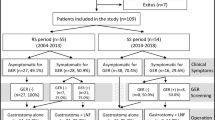
Thirty-two neurological impaired patients who underwent laparoscopic fundoplication and gastrostomy between 2015 and 2019 were classified into two groups based on stomach position: non-elevated stomach position (NESP) and elevated stomach position (ESP). Patients’ characteristics, operative result and postoperative gastric emptying were reviewed.
Results
The 11 ESP patients were significantly older than the 21 NESP patients (p < 0.05). The ESP patients had a significantly heavier body weight (BW) than the NESP patients (p < 0.05). The time taken (days) to reduce gastric drainage (days, below BW × 10 ml) in the NESP (4.3 ± 3.6) was significantly longer than that of ESP (1.3 ± 1.6) (p < 0.05). The time taken (days) to achieve full enteral nutrition in the NESP (14.1 ± 8.9) was significantly longer than that of the ESP patients (8.8 ± 3.1) (p < 0.05).
Conclusion
Elevated stomach position (ESP) patients archived full enteral nutrition earlier than NESP patients after laparoscopic fundoplication and gastrostomy. Stomach position correction might, therefore, be involved in the incidence of DGE.

Similar content being viewed by others

References
Sullivan PB. Gastrointestinal disorders in children with neurodevelopmental disabilities. Dev Disabil Res Rev. 2008;14(2):128–36.
Bais JE, Samsom M, Boudesteijn EA, van Rijk PP, Akkermans LM, Gooszen HG. Impact of delayed gastric emptying on the outcome of antireflux surgery. Ann Surg. 2001;234(2):139–46.
Lauriti G, Lisi G, Lelli Chiesa P, Zani A, Pierro A. Gastroesophageal reflux in children with neurological impairment: a systematic review and meta-analysis. Pediatr Surg Int. 2018;34(11):1139–49.
Fonkalsrud EW, Ament ME. Gastroesophageal reflux in childhood. Curr Probl Surg. 1996;33(1):1–70.
Mauritz FA, van Herwaarden-Lindeboom MY, Stomp W, Zwaveling S, Fischer K, Houwen RH, et al. The effects and efficacy of antireflux surgery in children with gastroesophageal reflux disease: a systematic review. J Gastrointest Surg. 2011;15(10):1872–8.
Alexander F, Wyllie R, Jirousek K, Secic M, Porvasnik S. Delayed gastric emptying affects outcome of Nissen fundoplication in neurologically impaired children. Surgery. 1997;122(4):690–7 (discussion 697–8).
Okuyama H, Urao M, Starr GA, Drongowski RA, Coran AG, Hirschl RB. A comparison of the efficacy of pyloromyotomy and pyloroplasty in patients with gastroesophageal reflux and delayed gastric emptying. J Pediatr Surg. 1997;32(2):316–9.
Pacilli M, Pierro A, Lindley KJ, Curry JI, Eaton S. Gastric emptying is accelerated following laparoscopic Nissen fundoplication. Eur J Pediatr Surg. 2008;18(6):395–7.
Tog C, Liu DS, Lim HK, Stiven P, Thompson SK, Watson D, et al. Risk factors for delayed gastric emptying following laparoscopic repair of very large hiatus hernias. BJS Open. 2017;1(3):75–8.
van Rijn S, Rinsma NF, van Herwaarden-Lindeboom MYA, Ringers J, Gooszen HG, van Rijn PJJ, et al. Effect of vagus nerve integrity on short and long-term efficacy of antireflux surgery. Am J Gastroenterol. 2016;111(4):508–15.
Harumatsu T, Nagai T, Yano K, Onishi S, Yamada K, Yamada W, et al. Differential advantage of liver retraction methods in laparoscopic fundoplication for neurologically impaired patients: a comparison of three kinds of procedures. Pediatr Surg Int. 2020;36(5):591–6.
Desai KM, Sessa WC, Vane JR. Involvement of nitric oxide in the reflex relaxation of the stomach to accommodate food or fluid. Nature. 1991;351(6326):477–9.
Wijnhoven BP, Salet GA, Roelofs JM, Smout AJ, Akkermans LM, Gooszen HG. Function of the proximal stomach after Nissen fundoplication. Br J Surg. 1998;85(2):267–71.
Kwiatek MA, Menne D, Steingoetter A, Goetze O, Forras-Kaufman Z, Kaufman E, et al. Effect of meal volume and calorie load on postprandial gastric function and emptying: studies under physiological conditions by combined fiber-optic pressure measurement and MRI. Am J Physiol Gastrointest Liver Physiol. 2009;297(5):G894-901.
Maddern GJ, Jamieson GG. Fundoplication enhances gastric emptying. Ann Surg. 1985;201(3):296–9.
Viljakka M, Saali K, Koskinen M, Karhumäki L, Kössi J, Luostarinen M, et al. Antireflux surgery enhances gastric emptying. Arch Surg. 1999;134(1):18–21.
Mousa H, Caniano DA, Alhajj M, Gibson L, Lorenzo CD, Binkowitz L. Effect of Nissen fundoplication on gastric motor and sensory functions. J Pediatr Gastroenterol Nutr. 2006;43(2):185–9.
Hinder RA, Stein HJ, Bremner CG, DeMeester TR. Relationship of a satisfactory outcome to normalization of delayed gastric emptying after Nissen fundoplication. Ann Surg. 1989;210(4):458–64.
Acknowledgements
We thank Mr. Brain Quinn for his comments and help with the manuscript. This study was supported by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JSPS, nos. 16K11350, 19K09150), research grant from JFE (The Japanese Foundation for Research and Promotion of Endoscopy), research grant from J-CASE (Japanese Consortium of Advanced Surgical Endoscopy), research grant from Kyushu Society of Endoscopic and Robotic Surgery, research grant of Karl Storz Award from Japan Society for Endoscopic Surgery, research grant from The Mother and Child Health Foundation, research grant from the Kawano Masanori Memorial Public Interest Incorporated Foundation for Promotion of Pediatrics, and Research Grant from Princess Takamatsu Cancer Research Fund.
Funding
No funding was received for this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No competing financial interests exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matsukubo, M., Kaji, T., Onishi, S. et al. Differential gastric emptiness according to preoperative stomach position in neurological impaired patients who underwent laparoscopic fundoplication and gastrostomy. Surg Today 51, 1918–1923 (2021). https://doi.org/10.1007/s00595-021-02274-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02274-w