Abstract
Purpose
The effectiveness of using anti-adhesion agents in laparoscopic surgery is controversial. We compared the outcomes of patients exposed to anti-adhesion agents (barrier group) with those of patients not exposed (no barrier group) in laparoscopic surgery.
Methods
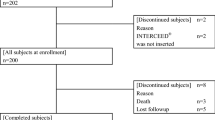
Using a nationwide claim-based database in Japan, we analyzed data from patients who underwent laparoscopic surgery between 2005 and 2019 and compared the patient characteristics and the proportion of those with bowel obstruction between the barrier and no barrier groups. We also performed several sensitivity and subgroup analyses.
Results
Of the 57,499 patients who met the inclusion criteria, 14,360 and 43,139 were assigned to the barrier and no barrier groups, respectively. The proportion of patients with a bowel obstruction in the two groups did not differ among all patients hospitalized for obstruction (1.1 vs. 1.1%, p = 0.63) and those requiring surgery (0.2 vs. 0.2%, p = 0.39). In the sensitivity analysis with propensity score matching, the incidences of bowel obstruction between the barrier and non-barrier groups were equivocal (1.3 vs. 1.6%), but statistically marginal (chi-square test, p = 0.035; log-rank test, p = 0.09).
Conclusion
The use of barrier agents for adhesive prevention did not show clear effectiveness for the prevention of bowel obstruction after laparoscopic surgery for unselected cases. Further studies focusing on more specific procedures are needed.


Similar content being viewed by others
References
Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353:1476–80.
Krielen P, Stommel MWJ, Pargmae P, Bouvy ND, Bakkum EA, Ellis H, et al. Adhesion-related readmissions after open and laparoscopic surgery: a retrospective cohort study (SCAR update). Lancet. 2020;395:33–41.
ten Broek RP, Issa Y, van Santbrink EJ, Bouvy ND, Kruitwagen RF, Jeekel J, et al. Burden of adhesions in abdominal and pelvic surgery: systematic review and met-analysis. BMJ. 2013. https://doi.org/10.1136/bmj.f5588.
Farinella E, Cirocchi R, La Mura F, Morelli U, Cattorini L, Delmonaco P, et al. Feasibility of laparoscopy for small bowel obstruction. World J Emerg Surg. 2009. https://doi.org/10.1186/1749-7922-4-3.
Miller G, Boman J, Shrier I, Gordon PH. Etiology of small bowel obstruction. Am J Surg. 2000;180:33–6.
Menzies D. Postoperative adhesions: their treatment and relevance in clinical practice. Ann R Coll Surg Engl. 1993;75:147–53.
Zeng Q, Yu Z, You J, Zhang Q. Efficacy and safety of Seprafilm for preventing postoperative abdominal adhesion: systematic review and meta-analysis. World J Surg. 2007;31:2125–31.
Kumar S, Wong PF, Leaper DJ. Intra-peritoneal prophylactic agents for preventing adhesions and adhesive intestinal obstruction after non-gynaecological abdominal surgery. Cochrane Database Syst Rev. 2009. https://doi.org/10.1002/14651858.CD005080.pub2.
Ten Broek RPG, Stommel MWJ, Strik C, van Laarhoven C, Keus F, van Goor H. Benefits and harms of adhesion barriers for abdominal surgery: a systematic review and meta-analysis. Lancet. 2014;383:48–59.
Ahmad G, Kim K, Thompson M, Agarwal P, O’Flynn H, Hindocha A, et al. Barrier agents for adhesion prevention after gynaecological surgery. Cochrane Database Syst Rev. 2020. https://doi.org/10.1002/14651858.CD000475.pub4.
Kim TN, Chung MK, Nam JK, Lee JZ, Chung JH, Lee SW. Effectiveness of hyaluronic acid/carboxymethylcellulose in preventing adhesive bowel obstruction after laparoscopic radical cystectomy. Asian J Surg. 2019;42:394–400.
Watanabe J, Ishida F, Ishida H, Fukunaga Y, Watanabe K, Naito M, et al. A prospective multi-center registry concerning the clinical performance of laparoscopic colorectal surgery using an absorbable adhesion barrier (INTERCEED(®)) made of oxidized regenerated cellulose. Surg Today. 2019;49:877–84.
Fujii S, Tsukamoto M, Shimada R, Okamoto K, Hayama T, Tsuchiya T, et al. Absorptive anti-adhesion barrier for the prevention of bowel obstruction after laparoscopic colorectal cancer surgery. J Anus Rectum Colon. 2018;2:1–8.
Ha US, Koh JS, Cho KJ, Yoon BI, Lee KW, Hong SH, et al. Hyaluronic acid-carboxymethylcellulose reduced postoperative bowel adhesions following laparoscopic urologic pelvic surgery: a prospective, randomized, controlled, single-blind study. BMC Urol. 2016;16:28. https://doi.org/10.1186/s12894-016-0149-3.
Naito M, Ogura N, Yamanashi T, Sato T, Nakamura T, Miura H, et al. Prospective randomized controlled study on the validity and safety of an absorbable adhesion barrier (Interceed®) made of oxidized regenerated cellulose for laparoscopic colorectal surgery. Asian J Endosc Surg. 2017;10:7–11.
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18:805–35.
Medical Information System Development Center (in Japanese). http://www2.medis.or.jp/stdcd/byomei/index.html. Accessed 11 Sep 2020.
Various Information of Medical Fee (in Japanese). https://shinryohoshu.mhlw.go.jp/shinryohoshu/kaitei/. Accessed 11 Sep 2020.
Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, Reijnen MM, Schaapveld M, Van Goor H. Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg. 2000;87:467–71.
ten Broek RP, Bakkum EA, Laarhoven CJ, van Goor H. Epidemiology and prevention of postsurgical adhesions revisited. Ann Surg. 2016;263:12–9.
Krielen P, Grutters JPC, Strik C, Ten Broek RPG, van Goor H, Stommel MWJ. Cost-effectiveness of the prevention of adhesions and adhesive small bowel obstruction after colorectal surgery with adhesion barriers: a modelling study. World J Emerg Surg. 2019. https://doi.org/10.1186/s13017-019-0261-2.
Dowson HM, Bong JJ, Lovell DP, Worthington TR, Karanjia ND, Rockall TA. Reduced adhesion formation following laparoscopic versus open colorectal surgery. Br J Surg. 2008;95:909–14.
Stommel MWJ, Ten Broek RPG, Strik C, Slooter GD, Verhoef C, Grünhagen DJ, et al. Multicenter observational study of adhesion formation after open-and laparoscopic surgery for colorectal cancer. Ann Surg. 2018;267:743–8.
Andersen P, Jensen KK, Erichsen R, Frøslev T, Krarup PM, Madsen MR, et al. Nationwide population-based cohort study to assess risk of surgery for adhesive small bowel obstruction following open or laparoscopic rectal cancer resection. BJS Open. 2017;1:30–8.
Tsuruta A, Itoh T, Hirai T, Nakamura M. Multi-layered intra-abdominal adhesion prophylaxis following laparoscopic colorectal surgery. Surg Endosc. 2015;29:1400–5.
Huang C, Ding DC. Outcomes of adhesion barriers in gynecologic surgeries: A retrospective study at a medical center. Medicine. 2019. https://doi.org/10.1097/md.0000000000018391.
Ohta S, Toda T, Inagaki F, Omichi K, Shimizu A, Kokudo N, et al. The Prevention of Hepatectomy-Induced Adhesions by Bilayer Sponge Composed of Ultrapure Alginate. J Surg Res. 2019;242:286–95.
Farquhar C, Vandekerckhove P, Watson A, Vail A, Wiseman D. Barrier agents for preventing adhesions after surgery for subfertility. Cochrane Database Syst Rev. 2000. https://doi.org/10.1002/14651858.Cd000475.
van der Wal JB, Iordens GI, Vrijland WW, van Veen RN, Lange J, Jeekel J. Adhesion prevention during laparotomy: long-term follow-up of a randomized clinical trial. Ann Surg. 2011;253:1118–21.
Sawada T, Nishizawa H, Nishio E, Kadowaki M. Postoperative adhesion prevention with an oxidized regenerated cellulose adhesion barrier in infertile women. J Reprod Med. 2000;45:387–9.
Beck DE, Opelka FG, Bailey HR, Rauh SM, Pashos CL. Incidence of small-bowel obstruction and adhesiolysis after open colorectal and general surgery. Dis Colon Rectum. 1999;42:241–8.
Strik C, Stommel MW, Schipper LJ, van Goor H, Ten Broek RP. Risk factors for future repeat abdominal surgery. Langenbecks Arch Surg. 2016;401:829–37.
Parker MC, Ellis H, Moran BJ, Thompson JN, Wilson MS, Menzies D, et al. Postoperative adhesions: ten-year follow-up of 12,584 patients undergoing lower abdominal surgery. Dis Colon Rectum. 2001;44:822–9.
Becker JM, Dayton MT, Fazio VW, Beck DE, Stryker SJ, Wexner SD, et al. Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized, double-blind multicenter study. J Am Coll Surg. 1996;183:297–306.
Vrijland WW, Tseng LN, Eijkman HJ, Hop WC, Jakimowicz JJ, Leguit P, et al. Fewer intraperitoneal adhesions with use of hyaluronic acid-carboxymethylcellulose membrane: a randomized clinical trial. Ann Surg. 2002;235:193–9.
Lee WS, Baek JH, Lee WK. Direct comparison of Seprafilm(R) versus Adept (R) versus no additive for reducing the risk of small-bowel obstruction in colorectal cancer surgery. Surg Today. 2013;43:995–1002.
Chuang YC, Lu HF, Peng FS, Ting WH, Tu FC, Chen MJ, et al. Modified novel technique for improving the success rate of applying seprafilm by using laparoscopy. J Minim Invasive Gynecol. 2014;21:787–90.
Huang YT, Su YY, Wu KY, Huang HY, Lin YS, Weng CH, et al. Learning curve analysis of applying Seprafilm hyaluronic acid/carboxymethylcellulose membrane during laparoscopic hysterectomy. Sci Rep. 2020. https://doi.org/10.1038/s41598-020-75523-6.
Hirschelmann A, Tchartchian G, Wallwiener M, Hackethal A, De Wilde RL. A review of the problematic adhesion prophylaxis in gynaecological surgery. Arch Gynecol Obstet. 2012;285:1089–97.
Rajab TK, Kimonis KO, Ali E, Offodile AC 2nd, Brady M, Bleday R. Practical implications of postoperative adhesions for preoperative consent and operative technique. Int J Surg. 2013;11:753–6.
DeWilde RL, Trew G, On behalf of the Expert Adhesions Working Party of the European Society of Gynaecological Endosopy (ESGE). Postoperative abdominal adhesions and their prevention in gynaecological surgery. Expert consensus position. Part 2—steps to reduce adhesions. Gynecol Surg. 2007;4:243–53.
Reed KL, Fruin AB, Bishop-Bartolomei KK, Gower AC, Nicolaou M, Stucchi AF, et al. Neurokinin-1 receptor and substance P messenger RNA levels increase during intraabdominal adhesion formation. J Surg Res. 2002;108:165–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
K.K. received an advisory fee from Shin Nippon Biomedical Laboratories, Ltd., JMDC Inc., AGREE Inc.; research funds from Sumitomo Dainippon Pharma Co, Ltd., Pfizer Inc., Stella Pharma Corporation, CMIC Co., Ltd., Suntory Beverage & Food Ltd., Medical Platform Co., Ltd., and Real World Data, Co., Ltd.; and holds stocks in Real World Data, Co., Ltd. There are no patent products under development or marketed products to declare relevant to these companies. M.N. and M.T. state that they have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nakashima, M., Takeuchi, M. & Kawakami, K. Effectiveness of barrier agents for preventing postoperative bowel obstruction after laparoscopic surgery: a retrospective cohort study. Surg Today 51, 1335–1342 (2021). https://doi.org/10.1007/s00595-021-02258-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02258-w