Abstract
Purpose
Surgical site infection (SSI) occurs at a high rate after ileostomy closure. The effect of preventive negative-pressure wound therapy (NPWT) on SSI development in closed wounds remains controversial. We conducted a prospective multicenter study to evaluate the usefulness of preventive NPWT for SSI after ileostomy closure.
Methods
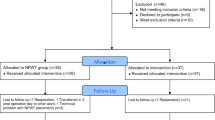
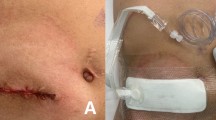
From January 2018 to November 2018, 50 patients who underwent closure of ileostomy created after surgery for colorectal cancer participated in this study. An NPWT device was applied to each wound immediately after surgery and then treatment was continued for 3 days. The primary endpoint was 30-day SSI, and the secondary endpoints were the incidence of seroma, hematoma, and adverse events related to NPWT.
Results
No patients developed SSI, seroma, or hematoma. Adverse events that may have been causally linked with NPWT were contact dermatitis in two patients and wound pain in one patient, and there were no cases of discontinuation or decompression of NPWT.
Conclusion
The use of NPWT following ileostomy closure may be useful for reducing the development of SSI in colorectal cancer patients. This is a prospective multicenter pilot study and we are planning a comparative study based on these successful results.
Trail registration
Registration number: UMIN000032053 (https://www.umin.ac.jp/).


Similar content being viewed by others
References
Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med. 1991;91(3b):152s–s157157.
Kashimura N, Kusachi S, Konishi T, Shimizu J, Kusunoki M, Oka M, et al. Impact of surgical site infection after colorectal surgery on hospital stay and medical expenditure in Japan. Surg Today. 2012;42(7):639–45.
Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1990s;20(11):725–30.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, Guideline for Prevention of Surgical Site Infection. Centers for disease control and prevention (CDC) hospital infection control practices advisory committee. Am J Infect Control. 1999;27(2):97–132 (quiz 3-4; discussion 96).
Yoshida K, Honda M, Kumamaru H, Kodera Y, Kakeji Y, Hiki N, et al. Surgical outcomes of laparoscopic distal gastrectomy compared to open distal gastrectomy: a retrospective cohort study based on a nationwide registry database in Japan. Ann Gastroenterol Surg. 2018;2(1):55–64.
Norman G, Atkinson RA, Smith TA, Rowlands C, Rithalia AD, Crosbie EJ, et al. Intracavity lavage and wound irrigation for prevention of surgical site infection. Cochrane Database Syst Rev. 2017;10:Cd012234.
Tsujinaka T, Yamamoto K, Fujita J, Endo S, Kawada J, Nakahira S, et al. Subcuticular sutures versus staples for skin closure after open gastrointestinal surgery: a phase 3, multicentre, open-label, randomised controlled trial. Lancet (London, England). 2013;382(9898):1105–12.
Gessler B, Haglind E, Angenete E. Loop ileostomies in colorectal cancer patients–morbidity and risk factors for nonreversal. J Surg Res. 2012;178(2):708–14.
Chun LJ, Haigh PI, Tam MS, Abbas MA. Defunctioning loop ileostomy for pelvic anastomoses: predictors of morbidity and nonclosure. Dis Colon Rectum. 2012;55(2):167–74.
Korol E, Johnston K, Waser N, Sifakis F, Jafri HS, Lo M, et al. A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS ONE. 2013;8(12):e83743.
van Westreenen HL, Visser A, Tanis PJ, Bemelman WA. Morbidity related to defunctioning ileostomy closure after ileal pouch-anal anastomosis and low colonic anastomosis. Int J Colorectal Dis. 2012;27(1):49–544.
Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38(6):563–76 (discussion 77).
Blackham AU, Farrah JP, McCoy TP, Schmidt BS, Shen P. Prevention of surgical site infections in high-risk patients with laparotomy incisions using negative-pressure therapy. Am J Surg. 2013;205(6):647–54.
Bonds AM, Novick TK, Dietert JB, Araghizadeh FY, Olson CH. Incisional negative pressure wound therapy significantly reduces surgical site infection in open colorectal surgery. Dis Colon Rectum. 2013;56(12):1403–8.
O'Leary DP, Peirce C, Anglim B, Burton M, Concannon E, Carter M, et al. Prophylactic negative pressure dressing use in closed laparotomy wounds following abdominal operations: a randomized, controlled, open-label trial: the P.I.C.O. trial. Annals Surg. 2017;265(6):1082–6.
Sahebally SM, McKevitt K, Stephens I, Fitzpatrick F, Deasy J, Burke JP, et al. Negative pressure wound therapy for closed laparotomy incisions in general and colorectal surgery: a systematic review and meta-analysis. JAMA Surg. 2018;153(11):e183467.
Cantero R, Rubio-Perez I, Leon M, Alvarez M, Diaz B, Herrera A, et al. Negative-pressure therapy to reduce the risk of wound infection following diverting loop ileostomy reversal: an initial study. Adv Skin wound care. 2016;29(3):114–8.
Poehnert D, Hadeler N, Schrem H, Kaltenborn A, Klempnauer J, Winny M. Decreased superficial surgical site infections, shortened hospital stay, and improved quality of life due to incisional negative pressure wound therapy after reversal of double loop ileostomy. Wound Repair Regen. 2017;25(6):994–1001.
Masden D, Goldstein J, Endara M, Xu K, Steinberg J, Attinger C. Negative pressure wound therapy for at-risk surgical closures in patients with multiple comorbidities: a prospective randomized controlled study. Ann Surg. 2012;255(6):1043–7.
Miyo M, Takemasa I, Ikeda M, Tujie M, Hasegawa J, Ohue M, et al. The influence of specific technical maneuvers utilized in the creation of diverting loop-ileostomies on stoma-related morbidity. Surg Today. 2017;47(8):940–50.
Ruiz-Tovar J, Alonso N, Morales V, Llavero C. Association between triclosan-coated sutures for abdominal wall closure and incisional surgical site infection after open surgery in patients presenting with fecal peritonitis: a randomized clinical trial. Surg Infect (Larchmt). 2015;16(5):588–94.
Nikfarjam M, Weinberg L, Fink MA, Muralidharan V, Starkey G, Jones R, et al. Pressurized pulse irrigation with saline reduces surgical-site infections following major hepatobiliary and pancreatic surgery: randomized controlled trial. World J Surg. 2014;38(2):447–55.
Kobayashi S, Ito M, Yamamoto S, Kinugasa Y, Kotake M, Saida Y, et al. Randomized clinical trial of skin closure by subcuticular suture or skin stapling after elective colorectal cancer surgery. Br J Surg. 2015;102(5):495–500.
Reid K, Pockney P, Pollitt T, Draganic B, Smith SR. Randomized clinical trial of short-term outcomes following purse-string versus conventional closure of ileostomy wounds. Br J Surg. 2010;97(10):1511–7.
Kim JJ, Franczyk M, Gottlieb LJ, Song DH. Cost-effective alternative for negative-pressure wound therapy. Plast Reconstr Surg Glob Open. 2017;5(2):e1211.
Kalady MF, Fields RC, Klein S, Nielsen KC, Mantyh CR, Ludwig KA. Loop ileostomy closure at an ambulatory surgery facility: a safe and cost-effective alternative to routine hospitalization. Dis Colon Rectum. 2003;46(4):486–90.
Banerjee A. Pursestring skin closure after stoma reversal. Dis Colon Rectum. 1997;40(8):993–4.
Lee JT, Marquez TT, Clerc D, Gie O, Demartines N, Madoff RD, et al. Pursestring closure of the stoma site leads to fewer wound infections: results from a multicenter randomized controlled trial. Dis Colon Rectum. 2014;57(11):1282–9.
O'Leary DP, Carter M, Wijewardene D, Burton M, Waldron D, Condon E, et al. The effect of purse-string approximation versus linear approximation of ileostomy reversal wounds on morbidity rates and patient satisfaction: the 'STOMA' trial. Tech Coloproctol. 2017;21(11):863–8.
Acknowledgements
We are grateful to Drs. M. Kimura (Saiseikai Otaru Hospital), J. Kimura (Hokkaido Ohno Memoriarl Hospital), M Nishimori (Sapporo Dohto Hospital), H Ohshima (Sapporo Teishinkai Hospital), and S. Son (Saiseikai Otaru Hospital) for their assistance in this study.
Funding
This research was carried out using research funds from the Sapporo Medical University. There was no financial support from any companies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Okuya, K., Takemasa, I., Tsuruma, T. et al. Evaluation of negative-pressure wound therapy for surgical site infections after ileostomy closure in colorectal cancer patients: a prospective multicenter study. Surg Today 50, 1687–1693 (2020). https://doi.org/10.1007/s00595-020-02068-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-02068-6