Abstract
Purpose
We investigated whether functional future remnant liver volume (fFRLV), assessed using gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging (EOB-MRI), could evaluate regional liver function in hepatocellular carcinoma (HCC) patients with portal vein tumor thrombus (PVTT) and help establish the indication for hepatectomy.
Methods
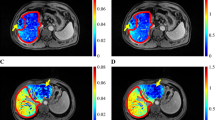
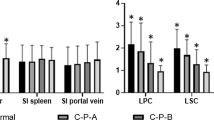
The subjects of this study were 12 patients with PVTT [PVTT(+) group] and 58 patients without PVTT [PVTT(−) group], from among 191 patients who underwent hepatectomy of more than one segment for HCC. We calculated the liver-to-muscle ratio (LMR) in the remnant liver, using EOB-MRI and fFRLV. Preoperative factors and surgical outcome were compared between the groups. The LMR of the area occluded by PVTT was compared with that of the non-occluded area.
Results
The indocyanine green retention rate at 15 min (ICG-R15) and liver fibrosis indices were increased in the PVTT(+) group, but the surgical outcomes of patients in this group were acceptable, with no liver failure, no mortality, and no differences from those in the PVTT(−) group. The fFRLV in the PVTT(+) group was not significantly different from that in the PVTT(−) group (p = 0.663). The LMR was significantly lower in the occluded area than in the non-occluded area (p = 0.004), indicating decreased liver function.
Conclusion
Assessing fFRLV using EOB-MRI could be useful for evaluating regional liver function and establishing operative indications for HCC with PVTT.




Similar content being viewed by others
References
Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379:1245–55. https://doi.org/10.1016/s0140-6736(11)61347-0.
Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology. 1999;29:62–7. https://doi.org/10.1002/hep.510290145.
Ikai I, Hatano E, Hasegawa S, Fujii H, Taura K, Uyama N, et al. Prognostic index for patients with hepatocellular carcinoma combined with tumor thrombosis in the major portal vein. J Am Coll Surg. 2006;202:431–8. https://doi.org/10.1016/j.jamcollsurg.2005.11.012.
Ban D, Shimada K, Yamamoto Y, Nara S, Esaki M, Sakamoto Y, et al. Efficacy of a hepatectomy and a tumor thrombectomy for hepatocellular carcinoma with tumor thrombus extending to the main portal vein. J Gastrointest Surg. 2009;13:1921–8. https://doi.org/10.1007/s11605-009-0998-0.
Matono R, Yoshiya S, Motomura T, Toshima T, Kayashima H, Masuda T, et al. Factors linked to longterm survival of patients with hepatocellular carcinoma accompanied by tumour thrombus in the major portal vein after surgical resection. HPB (Oxford). 2012;14:247–53. https://doi.org/10.1111/j.1477-2574.2011.00436.x.
Shi J, Lai EC, Li N, Guo WX, Xue J, Lau WY, et al. Surgical treatment of hepatocellular carcinoma with portal vein tumor thrombus. Ann Surg Oncol. 2010;17:2073–80. https://doi.org/10.1245/s10434-010-0940-4.
Ye JZ, Wang YY, Bai T, Chen J, Xiang BD, Wu FX, et al. Surgical resection for hepatocellular carcinoma with portal vein tumor thrombus in the Asia-Pacific region beyond the Barcelona Clinic Liver Cancer treatment algorithms: a review and update. Oncotarget. 2017;8:93258–78. https://doi.org/10.18632/oncotarget.18735.
Nishie A, Ushijima Y, Tajima T, Asayama Y, Ishigami K, Kakihara D, et al. Quantitative analysis of liver function using superparamagnetic iron oxide- and Gd-EOB-DTPA-enhanced MRI: comparison with Technetium-99 m galactosyl serum albumin scintigraphy. Eur J Radiol. 2012;81:1100–4. https://doi.org/10.1016/j.ejrad.2011.02.053.
Tajima T, Takao H, Akai H, Kiryu S, Imamura H, Watanabe Y, et al. Relationship between liver function and liver signal intensity in hepatobiliary phase of gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging. J Comput Assist Tomogr. 2010;34:362–6. https://doi.org/10.1097/RCT.0b013e3181cd3304.
Yamada A, Hara T, Li F, Fujinaga Y, Ueda K, Kadoya M, et al. Quantitative evaluation of liver function with use of gadoxetate disodium-enhanced MR imaging. Radiology. 2011;260:727–33. https://doi.org/10.1148/radiol.11100586.
Itoh S, Yoshizumi T, Shirabe K, Kimura K, Okabe H, Harimoto N, et al. Functional remnant liver assessment predicts liver-related morbidity after hepatic resection in patients with hepatocellular carcinoma. Hepatol Res. 2017;47:398–404. https://doi.org/10.1111/hepr.12761.
Araki K, Harimoto N, Kubo N, Watanabe A, Igarashi T, Tsukagoshi M, et al. Functional remnant liver volumetry using Gd-EOB-DTPA-enhanced magnetic resonance imaging (MRI) predicts post-hepatectomy liver failure in resection of more than one segment. HPB (Oxford). 2020;22:318–27. https://doi.org/10.1016/j.hpb.2019.08.002.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24. https://doi.org/10.1016/j.surg.2010.10.001.
Nishie A, Asayama Y, Ishigami K, Tajima T, Kakihara D, Nakayama T, et al. MR prediction of liver fibrosis using a liver-specific contrast agent: superparamagnetic iron oxide versus Gd-EOB-DTPA. J Magn Reson Imaging. 2012;36:664–71. https://doi.org/10.1002/jmri.23691.
Ninomiya M, Shirabe K, Kayashima H, Ikegami T, Nishie A, Harimoto N, et al. Functional assessment of the liver with gadolinium-ethoxybenzyl-diethylenetriamine penta-acetate-enhanced MRI in living-donor liver transplantation. Br J Surg. 2015;102:944–51. https://doi.org/10.1002/bjs.9820.
Nagino M, Kamiya J, Nishio H, Ebata T, Arai T, Nimura Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg. 2006;243:364–72. https://doi.org/10.1097/01.sla.0000201482.11876.14.
Shirabe K, Shimada M, Gion T, Hasegawa H, Takenaka K, Utsunomiya T, et al. Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg. 1999;188:304–9.
Jones RM, Moulton CE, Hardy KJ. Central venous pressure and its effect on blood loss during liver resection. Br J Surg. 1998;85:1058–60. https://doi.org/10.1046/j.1365-2168.1998.00795.x.
Iguchi T, Ikegami T, Fujiyoshi T, Yoshizumi T, Shirabe K, Maehara Y. Low positive airway pressure without positive end-expiratory pressure decreases blood loss during hepatectomy in living liver donors. Dig Surg. 2017;34:192–6. https://doi.org/10.1159/000447755.
Otsubo T, Takasaki K, Yamamoto M, Katsuragawa H, Katagiri S, Yoshitoshi K, et al. Bleeding during hepatectomy can be reduced by clamping the inferior vena cava below the liver. Surgery. 2004;135:67–73. https://doi.org/10.1016/s0039.
Rahbari NN, Koch M, Zimmermann JB, Elbers H, Bruckner T, Contin P, et al. Infrahepatic inferior vena cava clamping for reduction of central venous pressure and blood loss during hepatic resection: a randomized controlled trial. Ann Surg. 2011;253:1102–10. https://doi.org/10.1097/SLA.0b013e318214bee5.
Miyagawa S, Makuuchi M, Kawasaki S, Kakazu T. Criteria for safe hepatic resection. Am J Surg. 1995;169:589–94.
Imamura H, Seyama Y, Kokudo N, Maema A, Sugawara Y, Sano K, et al. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg. 2003;138:1198–206. https://doi.org/10.1001/archsurg.138.11.1198(discussion 206).
Kubota K, Makuuchi M, Kusaka K, Kobayashi T, Miki K, Hasegawa K, et al. Measurement of liver volume and hepatic functional reserve as a guide to decision-making in resectional surgery for hepatic tumors. Hepatology. 1997;26:1176–81. https://doi.org/10.1053/jhep.1997.v26.pm0009362359.
Shoup M, Gonen M, D’Angelica M, Jarnagin WR, DeMatteo RP, Schwartz LH, et al. Volumetric analysis predicts hepatic dysfunction in patients undergoing major liver resection. J Gastrointest Surg. 2003;7:325–30.
Kwon AH, Ha-Kawa SK, Uetsuji S, Inoue T, Matsui Y, Kamiyama Y. Preoperative determination of the surgical procedure for hepatectomy using technetium-99 m-galactosyl human serum albumin (99 mTc-GSA) liver scintigraphy. Hepatology. 1997;25:426–9. https://doi.org/10.1002/hep.510250228.
Hayashi H, Beppu T, Okabe H, Kuroki H, Nakagawa S, Imai K, et al. Functional assessment versus conventional volumetric assessment in the prediction of operative outcomes after major hepatectomy. Surgery. 2015;157:20–6. https://doi.org/10.1016/j.surg.2014.06.013.
Utsunomiya T, Shimada M, Hanaoka J, Kanamoto M, Ikemoto T, Morine Y, et al. Possible utility of MRI using Gd-EOB-DTPA for estimating liver functional reserve. J Gastroenterol. 2012;47:470–6. https://doi.org/10.1007/s00535-011-0513-8.
Morine Y, Enkhbold C, Imura S, Ikemoto T, Iwahashi S, Saito YU, et al. Accurate estimation of functional liver volume using Gd-EOB-DTPA MRI compared to MDCT/(99m)Tc-SPECT fusion imaging. Anticancer Res. 2017;37:5693–700. https://doi.org/10.21873/anticanres.12006.
Acknowledgments
We thank H. Tanaka, K. Hagiwara, K. Hoshino, and R. Muranushi for collecting data that formed the basis of this study. We also thank K. Ujita and J. Fukuda for their special assistance in image analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Fig.
1. Correlation scatter plots between functional future remnant liver volume (fFRLV) and ICG-Krem and between fFRLV and functional %RLV of 3D-CT/SPECT fusion in the PVTT(+) group.(a) Correlation of fFRLV and ICG-Krem in the PVTT(+) group. (b) Correlation of fFRLV and functional %RLV of 3D-CT/SPECT fusion in the PVTT(+) group
Rights and permissions
About this article
Cite this article
Araki, K., Harimoto, N., Yamanaka, T. et al. Efficiency of regional functional liver volume assessment using Gd-EOB-DTPA-enhanced magnetic resonance imaging for hepatocellular carcinoma with portal vein tumor thrombus. Surg Today 50, 1496–1506 (2020). https://doi.org/10.1007/s00595-020-02062-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-02062-y