Abstract
Purpose
Conventional mitral valve replacement is associated with the loss of natural continuity of the mitral valve complex. This study evaluated the morphologic/histological characteristics and function of a decellularized mitral valve used as a transplantable graft.
Methods
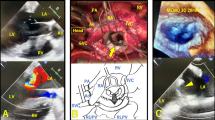
Hearts excised from pigs were decellularized by perfusion using detergent. Grafts with the mitral annulus, valve, chordae, and papillary muscle isolated from the decellularized heart were then transplanted into recipient pigs. After transplantation, the function of the graft was analyzed through echocardiography. A histological analysis was performed to evaluate the postoperative features of the decellularized graft.
Results
The decellularized graft was successfully transplanted in all cases but one. The remaining grafts maintained their morphology and function. They did not exhibit mitral regurgitation or stenosis. Only one animal survived for 3 weeks, and a histological analysis was able to be performed in this case. The transplanted valve was re-covered with endothelial cells. The microvessels in the papillary muscle were recellularized with vascular endothelial cells, and the papillary muscle was completely attached to the papillary muscle of the recipient.
Conclusion
The early outcome of decellularized mitral graft transplantation was acceptable. This native organ-derived acellular scaffold is a promising candidate for the replacement of the mitral valve complex.






Similar content being viewed by others
References
Masuda M, Endo S, Natsugoe S, Shimizu H, Doki Y, Hirata Y, et al. Thoracic and cardiovascular surgery in Japan during 2015: annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2018;66(10):581–615.
Lazam S, Vanoverschelde JL, Tribouilloy C, Grigioni F, Suri RM, Avierinos JF, et al. Twenty-year outcome after mitral repair versus replacement for severe degenerative mitral regurgitation: analysis of a large, prospective, multicenter international registry. Circulation. 2017;135(5):410–22.
Crapo PM, Gilbert TW, Badylak SF. An overview of tissue and whole organ decellularization processes. Biomaterials. 2011;32(12):3233–43.
Ott HC, Matthiesen TS, Goh SK, Black LD, Kren SM, Netoff TI, et al. Perfusion-decellularized matrix: using nature's platform to engineer a bioartificial heart. Nat Med. 2008;14(2):213–21.
Weymann A, Loganathan S, Takahashi H, Schies C, Claus B, Hirschberg K, et al. Development and evaluation of a perfusion decellularization porcine heart model. Circ J. 2011;75(4):852–60.
Momtahan N, Sukavaneshvar S, Roeder BL, Cook AD. Strategies and processes to decellularize and recellularize hearts to generate functional organs and reduce the risk of thrombosis. Tissue Eng Part B Rev. 2015;21(1):115–32.
Kitahara H, Yagi H, Tajima K, Okamoto K, Yoshitake A, Aeba R, et al. Heterotopic transplantation of a decellularized and recellularized whole porcine heart. Interact Cardiovasc Thorac Surg. 2016;22(5):571–9.
Yagi H, Fukumitsu K, Fukuda K, Kitago M, Shinoda M, Obara H, et al. Human-scale whole-organ bioengineering for liver transplantation: a regenerative medicine approach. Cell Transplant. 2013;22(2):231–42.
Katsuki Y, Yagi H, Okitsu T, Kitago M, Tajima K, Kadota Y, et al. Endocrine pancreas engineered using porcine islets and partial pancreatic scaffolds. Pancreatology. 2016;16(5):922–30.
da Costa FDA, Etnel JRG, Charitos EI, Sievers HH, Stierle U, Fornazari D, et al. Decellularized versus standard pulmonary allografts in the ross procedure: propensity-matched analysis. Ann Thorac Surg. 2018;105(4):1205–13.
Etnel JRG, Suss PH, Schnorr GM, Veloso M, Colatusso DF, Balbi Filho EM, et al. Fresh decellularized versus standard cryopreserved pulmonary allografts for right ventricular outflow tract reconstruction during the Ross procedure: a propensity-matched study. Eur J Cardiothorac Surg. 2018;54(3):434–40.
da Costa FDA, Etnel JRG, Torres R, Balbi Filho EM, Torres R, Calixto A, et al. Decellularized allografts for right ventricular outflow tract reconstruction in children. World J Pediatr Congenit Heart Surg. 2017;8(5):605–12.
Iablonskii P, Cebotari S, Ciubotaru A, Sarikouch S, Hoeffler K, Hilfiker A, et al. Decellularized mitral valve in a long-term sheep model. Eur J Cardiothorac Surg. 2018;53(6):1165–72.
Rabkin-Aikawa E, Farber M, Aikawa M, Schoen FJ. Dynamic and reversible changes of interstitial cell phenotype during remodeling of cardiac valves. The Journal of heart valve disease. 2004;13(5):841–7.
Rastelli GC. Evaluation of function of mital valve after homotransplantation in the dog. J Thorac Cardiovasc Surg. 1965;49:459–74.
Osako M, Hattori R, Nakao Y, Yamamura T, Fujii H, Otani H, et al. Freehand cryopreserved mitral valve allograft with flexible ring in the pig. Jpn J Thorac Cardiovasc Surg. 2000;48(12):775–81.
Acar C, Tolan M, Berrebi A, Gaer J, Gouezo R, Chauvaud S, et al. Homograft replacemnet of the mitral valve, Graft selection, technique of implantation, and result in 43 patients. J Thorac Cardiovasc Surg. 1994;111:367–80.
Shaddy RE, Hunter DD, Osbom KA, Lambert LM, Minich LL, Hawkins JA, et al. Prospective analysis of HLA immunogenicity of cryopreserved valved allografts used in pediatric heart surgery. Circulation. 1996;94(5):1063–7.
Roger JF, Baskett MA, Maurice A, Nanton MB, Andrew E, Warren MS, et al. Human leukocyte antigen-DR and ABO mismatch are associated with accelerated homograft valve failure in children: Implication for therapeutic interventions. J Thorac Cardiovasc Surg. 2003;126(1):232–8.
Ueno T, Ozawa H, Taira M, Kanaya T, Toda K, Kuratani T, et al. Pulmonary valve replacement with fresh decellularized pulmonary allograft for pulmonary regurgitation after tetralogy of fallot repair- first case report in Japan. Circ J. 2016;80(4):1041–3.
Sarikouch S, Horke A, Tudorache I, Beerbaum P, Westhoff-Bleck M, Boethig D, et al. Decellularized fresh homografts for pulmonary valve replacement: a decade of clinical experience. Eur J Cardiothorac Surg. 2016;50(2):281–90.
Neumann A, Sarikouch S, Breymann T, Cebotari S, Boethig D, Horke A, et al. Early systemic cellular immune response in children and young adults receiving decellularized fresh allografts for pulmonary valve replacement. Tissue Eng Part A. 2014;20(5–6):1003–111.
Kneib C, von Glehn CQ, Costa FD, Costa MT, Susin MF. Evaluation of humoral immune response to donor HLA after implantation of cellularized versus decellularized human heart valve allografts. Tissue Antigens. 2012;80(2):165–74.
Grabow N. Mechanical and structual properties of a novel hybrid heart valve scaffold for tissue engineering. Artif Organs. 2004;28(11):971–9.
Roy S, Silacci P, Stergiopulos N. Biomechanical properties of decellularized porcine common carotid arteries. Am J Physiol Heart Circ Physiol. 2005;289(4):H1567–1576.
Mirsadraee S. Development and characterization of an acellular human pericardial Matrix for tissue engineering. Tissue Eng. 2006;12(4):763–73.
Momtahan N, Poornejad N, Struk JA, Castleton AA, Herrod BJ, Vance BR, et al. Automation of pressure control improves whole porcine heart decellularization. Tissue Eng Part C Methods. 2015;21(11):1148–61.
Robertson MJ, Dries-Devlin JL, Kren SM, Burchfield JS, Taylor DA. Optimizing recellularization of whole decellularized heart extracellular matrix. PLoS ONE. 2014;9(2):e90406.
Acknowledgements
The authors thank Hitoshi Inoue and Shintaro Hashiba from Sasazuka Animal Clinic; Yosuke Kawahira and Shingo Sato from the Division of Clinical Engineering; Toshio Otake, Koji Matsumoto and Keiko Kumagai from the Laboratory Animal Center; Shinsuke Shibata, Toshihiro Nagai from the Department of Electron Microscope Laboratory; Naho Murakawa, Rie Kinoshita from the Department of Surgery; So Takasugi, Yusuke Aoki, Tadafumi Tamura and Kaori Katsumata from the Department of Cardiovascular Surgery, School of Medicine, Keio University.
Funding
This work was supported by JSPS KAKENHI Grant number JP 18K08582.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yu Inaba and the other co-authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Supplementary file2 (MP4 7213 kb)
Supplementary file3 (MP4 5112 kb)
Supplementary file4 (MP4 7621 kb)
Rights and permissions
About this article
Cite this article
Inaba, Y., Yagi, H., Kuroda, K. et al. Transplantation of a decellularized mitral valve complex in pigs. Surg Today 50, 298–306 (2020). https://doi.org/10.1007/s00595-019-01869-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-019-01869-8