Abstract
Purpose
We compared the outcomes of laparoscopic surgery (LS) with those of open surgery (OS) for unilateral and bilateral pediatric inguinal hernia.
Methods
Using a nationwide claim-based database in Japan, we analyzed data from children younger than 15 years old, who underwent inguinal hernia repair between January 2005 and December 2017. Patient characteristics, incidence of reoperation, postoperative complications, length of hospital stay, and duration of anesthesia were compared between LS and OS for unilateral and bilateral hernia.
Results
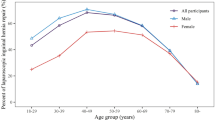
Among 5554 patients, 2057 underwent LS (unilateral 1095, bilateral 962) and 3497 underwent OS (unilateral 3177, bilateral 320). The incidence of recurrence was not significantly different between OS and LS (unilateral: OS 0.2% vs. LS 0.3%, p = 0.44, bilateral: OS 0.6% vs. LS 0.6%, p = 1.00). The incidence of metachronous hernias was significantly higher in the OS group than in the LS group (4.8% vs. 1.0%, p < 0.001). The surgical site infection rate was significantly lower after OS than after LS for unilateral surgeries (0.9% vs. 2.2%, p = 0.002). There was no difference between OS and LS in the length of hospital stay.
Conclusion
Both OS and LS had a low incidence of recurrence in children; however, the incidence of metachronous hernias was lower for LS, which may influence operative technique decisions.

Similar content being viewed by others
References
Chang YT, Lin JY, Lee JY, Tsai CJ, Chiu WC, Chiu CS. Comparative mid-term results between inguinal herniotomy and single-port laparoscopic herniorrhaphy for pediatric inguinal hernia. Surg Laparosc Endosc Percutan Tech. 2012;22:526–31.
Antonoff MB, Kreykes NS, Saltzman DA, Acton RD. American Academy of Pediatrics Section on Surgery hernia survey revisited. J Pediatr Surg. 2005;40:1009–144.
Bronsther B, Abrams MW, Elboim C. Inguinal hernias in children—a study of 1000 cases and a review of the literature. J Am Med Womens Assoc. 1972;1972(27):522–5.
Chang SJ, Chen JY, Hsu CK, Chuang FC, Yang SS. The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia. 2016;20:559–63.
Pogorelic Z, Rikalo M, Jukic M, Katic J, Juric I, Furlan D, et al. Modified Marcy repair for indirect inguinal hernia in children: a 24-year single-center experience of 6826 pediatric patients. Surg Today. 2017;47:108–13.
Erdogan D, Karaman I, Aslan MK, Karaman A, Cavusoglu YH. Analysis of 3776 pediatric inguinal hernia and hydrocele cases in a tertiary center. J Pediatr Surg. 2013;48:1767–72.
Takehara H, Yakabe S, Kameoka K. Laparoscopic percutaneous extraperitoneal closure for inguinal hernia in children: clinical outcome of 972 repairs done in three pediatric surgical institutions. J Pediatr Surg. 2006;41:1999–2003.
Endo M, Watanabe T, Nakano M, Yoshida F, Ukiyama E. Laparoscopic completely extraperitoneal repair of inguinal hernia in children: a single-institute experience with 1257 repairs compared with cut-down herniorrhaphy. Surg Endosc. 2009;23:1706–12.
Schier F. Laparoscopic inguinal hernia repair-a prospective personal series of 542 children. J Pediatr Surg. 2006;41:1081–4.
McClain L, Streck C, Lesher A, Cina R, Hebra A. Laparoscopic needle-assisted inguinal hernia repair in 495 children. Surg Endosc. 2015;29:781–6.
Miyake H, Fukumoto K, Yamoto M, Nouso H, Kaneshiro M, Nakajima H, et al. Comparison of percutaneous extraperitoneal closure (LPEC) and open repair for pediatric inguinal hernia: experience of a single institution with over 1000 cases. Surg Endosc. 2016;30:1466–72.
Amano H, Tanaka Y, Kawashima H, Deie K, Fujiogi M, Suzuki K, et al. Comparison of single-incision laparoscopic percutaneous extraperitoneal closure (SILPEC) and open repair for pediatric inguinal hernia: a single-center retrospective cohort study of 2028 cases. Surg Endosc. 2017;31:4988–95.
Esposito C, Escolino M, Cortese G, Aprea G, Turra F, Farina A, et al. Twenty-year experience with laparoscopic inguinal hernia repair in infants and children: considerations and results on 1833 hernia repairs. Surg Endosc. 2017;31:1461–8.
Zhao J, Chen Y, Lin J, Jin Y, Yang H, Wang F, et al. Potential value of routine contralateral patent processus vaginalis repair in children with unilateral inguinal hernia. Br J Surg. 2017;104:148–51.
Chan KL, Hui WC, Tam PK. Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc. 2005;19:927–32.
Tsai YC, Wu CC, Yang SS. Open versus minilaparoscopic herniorrhaphy for children: a prospective comparative trial with midterm follow-up evaluation. Surg Endosc. 2010;24:21–4.
Yang C, Zhang H, Pu J, Mei H, Zheng L, Tong Q. Laparoscopic vs open herniorrhaphy in the management of pediatric inguinal hernia: a systemic review and meta-analysis. J Pediatr Surg. 2011;46:1824–34.
Jun Z, Juntao G, Shuli L, Li L. A comparative study on trans-umbilical single-port laparoscopic approach versus conventional repair for incarcerated inguinal hernia in children. J Minim Access Surg. 2016;12:139–42.
Gause CD, Casamassima MG, Yang J, Hsiung G, Rhee D, Salazar JH, et al. Laparoscopic versus open inguinal hernia repair in children %3c/=3: a randomized controlled trial. Pediatr Surg Int. 2017;33:367–76.
Raveenthiran V, Agarwal P. Choice of repairing inguinal hernia in children: open versus laparoscopy. Indian J Pediatr. 2017;84:555–63.
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18:805–35.
Medical Information System Development Center. https://www2.medis.or.jp/stdcd/byomei/index.html. Accessed 22 Feb 2019 (in Japanese).
Wang F, Zhong H, Chen Y, Zhao J, Li Y, Chen J, et al. Single-site laparoscopic percutaneous extraperitoneal closure of the internal ring using an epidural and spinal needle: excellent results in 1464 children with inguinal hernia/hydrocele. Surg Endosc. 2017;31:2932–8.
Saranga Bharathi R, Arora M, Baskaran V. Pediatric inguinal hernia: laparoscopic versus open surgery. JSLS. 2008;12:277–81.
Koivusalo AI, Korpela R, Wirtavuori K, Piiparinen S, Rintala RJ, Pakarinen MP. A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics. 2009;123:332–7.
Shalaby R, Ibrahem R, Shahin M, Yehya A, Abdalrazek M, Alsayaad I, et al. Laparoscopic hernia repair versus open herniotomy in children: a controlled randomized study. Minim Invasive Surg. 2012;5:5. https://doi.org/10.1155/2012/484135.
Celebi S, Uysal AI, Inal FY, Yildiz A. A single-blinded, randomized comparison of laparoscopic versus open bilateral hernia repair in boys. J Laparoendosc Adv Surg Tech A. 2014;24:117–21.
Chan YY, Durbin-Johnson B, Kurzrock EA. Pediatric inguinal and scrotal surgery—practice patterns in US academic centers. J Pediatr Surg. 2016;51:1786–90.
Fujiogi M, Michihata N, Matsui H, Fushimi K, Yasunaga H, Fujishiro J. Outcomes following laparoscopic versus open surgery for pediatric inguinal hernia repair: Analysis using a national inpatient database in Japan. J Pediatr Surg. 2019;54:577–81.
Abd-Alrazek M, Alsherbiny H, Mahfouz M, Alsamahy O, Shalaby R, Shams A, et al. Laparoscopic pediatric inguinal hernia repair: a controlled randomized study. J Pediatr Surg. 2017;52:1539–44.
Endo M. Surgical repair of pediatric indirect inguinal hernia: great waves of change from open to laparoscopic approach. J Surg Transpl Sci. 2016. https://www.jscimedcentral.com/Surgery/surgery-4-1034.pdf.
Schier F, Montupet P, Esposito C. Laparoscopic inguinal herniorrhaphy in children: a three-center experience with 933 repairs. J Pediatr Surg. 2002;37:395–7.
Chinnaswamy P, Malladi V, Jani KV, Parthasarthi R, Shetty RA, Kavalakat AJ, et al. Laparoscopic inguinal hernia repair in children. JSLS. 2005;9:393–8.
Saka R, Okuyama H, Sasaki T, Nose S, Yoneyama C. Safety and efficacy of laparoscopic percutaneous extraperitoneal closure for inguinal hernias and hydroceles in children: a comparison with traditional open repair. J Laparoendosc Adv Surg Tech A. 2014;24:55–8.
Obata S, Ieiri S, Jimbo T, Souzaki R, Hashizume M, Taguchi T. Feasibility of single-incision laparoscopic percutaneous extraperitoneal closure for inguinal hernia by inexperienced pediatric surgeons: single-incision versus multi-incision randomized trial for 2 years. J Laparoendosc Adv Surg Tech A. 2016;26:218–21.
Taylor K, Sonderman KA, Wolf LL, Jiang W, Armstrong LB, Koehlmoos TP, et al. Hernia recurrence following inguinal hernia repair in children. J Pediatr Surg. 2018;53:2214–8.
Lee DY, Baik YH, Kwak BS, Oh MG, Choi WY. A purse-string suture at the level of internal inguinal ring, taking only the peritoneum leaving the distal sac: is it enough for inguinal hernia in pediatric patients? Hernia. 2015;19:607–10.
Lee SR, Choi SB. The efficacy of laparoscopic intracorporeal linear suture technique as a strategy for reducing recurrences in pediatric inguinal hernia. Hernia. 2017;21:425–33.
Lin J, Li D, Chen J, Lin L, Xu Y. Inguinal hernia repair by Bianchi incision in boys: a retrospective study. Pediatr Surg Int. 2018;34:289–95.
Zhu LL, Xu WJ, Liu JB, Huang X, Lv ZB. Comparison of laparoscopic hernia repair and open herniotomy in children: a retrospective cohort study. Hernia. 2017;21:417–23.
Ron O, Eaton S, Pierro A. Systematic review of the risk of developing a metachronous contralateral inguinal hernia in children. Br J Surg. 2007;94:804–11.
Shehata S, Shehata S, Wella HL, Abouheba M, Elrouby A. Pediatric inguinal hernias, are they all the same? A proposed pediatric hernia classification and tailored treatment. Hernia. 2018;22:941–6.
Esposito C, St Peter SD, Escolino M, Juang D, Settimi A, Holcomb GW 3rd. Laparoscopic versus open inguinal hernia repair in pediatric patients: a systematic review. J Laparoendosc Adv Surg Tech A. 2014;24:811–8.
Acknowledgements
We thank Dr. Masato Takeuchi for advice about revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K.K. received research funding from Olympus Corporation. M.N. and K.I. have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Online resource 1
MEDIS-DC codes for complications (DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Nakashima, M., Ide, K. & Kawakami, K. Laparoscopic versus open repair for inguinal hernia in children: a retrospective cohort study. Surg Today 49, 1044–1050 (2019). https://doi.org/10.1007/s00595-019-01847-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-019-01847-0