Abstract
Purpose
To investigate the impact of the pelvic dimensions and tumor volume on surgery in locally advanced rectal cancer.
Methods
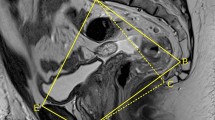
Patients who underwent open surgery after neoadjuvant long-course chemoradiation for primary rectal cancer were included. The predictive value of magnetic resonance-based pelvic measurements and tumor volume on the surgical difficulty and oncologic outcome were analyzed.
Results
125 patients were included. The independent risk factors related to the circumferential resection margin status were the pT stage [odds ratio (OR) 3.64, confidence interval (CI) 1.409–7.327] and tumor volume after neoadjuvant chemoradiotherapy (OR 1.59, CI 1.018–2.767). The operative time (p = 0.014, OR 1.453) and pelvic depth (p = 0.023, OR 1.116) were independent predictive factors for anastomotic leak. The median follow-up was 72 (2–113) months. Local recurrence was seen in 17 (14.1%) patients. Anastomotic leak (OR 1.799, CI 0.978–3.277), the circumferential resection margin status (OR 3.217, CI 1.262–7.870) and the relative tumor volume rate (OR 1.260, CI 1.004–1.912) were independent prognosticators of local recurrence. The 5-year overall survival was 66.7%. The circumferential resection margin status (hazard ratio: 4.739, CI 2.276–9.317), pN stage (OR 3.267, CI 1.195–8.930) and relative tumor volume rate (OR 2.628, CI 1.042–6.631) were independent prognostic factors for the overall survival.
Conclusions
Relative dimensions of the tumor in the pelvis influence the local recurrence and overall survival rates. Magnetic resonance-based measurements can predict the difficulty of surgery and allow surgeons to consider the appropriate surgical approach.


Similar content being viewed by others
References
Kornprat P, Pollheimer MJ, Lindtner RA, Schlemmer A, Rehak P, Langner C. Value of tumor size as a prognostic variable in colorectal cancer: a critical reappraisal. Am J Clin Oncol. 2011;34(1):43–9.
Crozier JE, McMillan DC, McArdle CS, Angerson WJ, Anderson JH, Horgan PG, et al. Tumor size is associated with the systemic inflammatory response but not survival in patients with primary operable colorectal cancer. J Gastroenterol Hepatol. 2007;22(12):2288–91.
Trakarnsanga A, Gonen M, Shia J, Goodman KA, Nash GM, Temple LK, et al. What is the significance of the circumferential margin in locally advanced rectal cancer after neoadjuvant chemoradiotherapy? Ann Surg Oncol. 2013;20(4):1179–84.
Baik SH, Kim NK, Lee KY, Sohn SK, Cho CH, et al. Factors influencing pathologic results after total mesorectal excision for rectal cancer: analysis of consecutive 100 cases. Ann Surg Oncol. 2008;15(3):721–8.
Quirke P, Durdey P, Dixon M, Williams N. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Lancet. 1986;2(8514):996–9.
Leonard D, Penninckx F, Fieuws S, Jouret-Mourin A, Sempoux C, Jehaes C, et al. Factors predicting the quality of total mesorectal excision for rectal cancer. Ann Surg. 2010;252(6):982–8.
Quirke P, Dixon MF. The prediction of local recurrence in rectal adenocarcinoma by histopathological examination. Int J Colorectal Dis. 1988;3(2):127–31. https://doi.org/10.1007/BF01645318.
Wibe A, Rendedal P. Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg. 2002;98(8):327–34.
Curvo-Semedo L, Lambregts DM, Maas M, Thywissen T, Mehsen RT, Lammering G, et al. Rectal cancer: assessment of complete response to preoperative combined radiation therapy with chemotherapy–conventional MR volumetry versus diffusion-weighted MR imaging. Radiology. 2011;260(3):734–43.
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery. 2010;147(3):339–51.
Salerno G, Daniels IR, Brown G, Heald RJ, Moran BJ. Magnetic resonance imaging pelvimetry in 186 patients with rectal cancer confirms an overlap in pelvic size between males and females. Colorectal Dis. 2006;8(9):772–6.
Boyle KM, Petty D, Chalmers G, Quirke P, Cairns A, Finan PJ, et al. MRI assessment of the bony pelvis may help predict resectability of rectal cancer. Colorectal Dis. 2005;7(3):232–40.
Kim CW, Baek SJ, Hur H, Min BS, Baik SH, Kim NK. Anastomotic leakage after low anterior resection for rectal cancer is different between minimally invasive surgery and open surgery. Ann Surg. 2006;263(1):130–7.
National Comprehensive CancerNetwork (2017) Rectal Cancer. (Version 3. 2017). https://www.nccn.org/professionals/physician_gls/pdf/rectal_blocks.pdf.
Bogach J, Tsai S, Zbuk K, Wong R, Grubac V, Coates A, et al. Quality of preoperative pelvic computed tomography (CT) and magnetic resonance imaging (MRI) for rectal cancer in a region in Ontario: a retrospective population-based study. J Surg Oncol. 2018;117(5):1038–42.
Can CT. Replace MRI in preoperative assessment of the circumferential resection margin in rectal cancer? Dis Colon Rectum. 2010;53(3) 308–14.
Nasseri Y, Langenfeld SJ. Imaging for colorectal cancer. Surg Clin North Am. 2017;97(3):503–13.
Akiyoshi T, Watanabe T, Ueno M. Pelvic dimensions as a predictor of difficulty in laparoscopic surgery for rectal cancer. Surg Endosc. 2011;25(9):3122–3.
Killeen T, Banerjee S, Vijay V, Al-Dabbagh Z, Francis D, Warren S. Pelvic dimensions as a predictor of difficulty in laparoscopic surgery for rectal cancer. Surg Endosc. 2012;26(1):277.
Ogiso S, Yamaguchi T, Hata H, Fukuda M, Ikai I, Yamato T. Evaluation of factors affecting the difficulty of laparoscopic anterior resection for rectal cancer: “narrow pelvis” is not a contraindication. Surg Endosc. 2011;25(6):1907–12.
Bertani E, Chiappa A, Della Vigna P, Radice D, Papis D, Cossu L, Biffi R, et al. The Impact of pelvimetry on anastomotic leakage in a consecutive series of open, laparoscopic and robotic low anterior resections with total mesorectal excision for rectal cancer. Hepatogastroenterology. 2014;61(134):1574–81.
Yeo SG, Kim DY, Kim TH, Jung KH, Hong YS, Chang HJ, Park JW, et al. Tumor volume reduction rate measured by magnetic resonance volumetry correlated with pathologic tumor response of preoperative chemoradiotherapy for rectal cancer. Int J Radiat Oncol Biol Phys. 2010;78(1):164–71.
Young HK, Dae YK, Tae HK, Jung KH, Chang HJ, Jeong SY, et al. Usefulness of magnetic resonance volumetric evaluation in predicting response to preoperative concurrent chemoradiotherapy in patients with resectable rectal cancer. Int J Radiat Oncol Biol Phys. 2005;62(3):761–8.
Lambrecht M, Vandecaveye V, De Keyzer F, Roels S, Penninckx F, Van Cutsem E, et al. Value of diffusion-weighted magnetic resonance imaging for prediction and early assessment of response to neoadjuvant radiochemotherapy in rectal cancer: preliminary results. Int J Radiat Oncol Biol Phys. 2012;82(2):863–70.
Lee Y-C, Hsieh C-C, Chuang J-P. Prognostic significance of partial tumor regression after preoperative chemoradiotherapy for rectal cancer: a meta-analysis. Dis Colon Rectum. 2013;56(9):1093–101.
Nougaret S, Rouanet P, Molinari N, Pierredon MA, Bibeau F, Azria D, et al. MR volumetric measurement of low rectal cancer helps predict tumor response and outcome after combined chemotherapy and radiation therapy. Radiology. 2012;263(2):409–18.
Poritz LS, Sehgal R, Hartnett K, Berg A, Koltun WA. Tumor volume and percent positive lymph nodes as a predictor of 5-year survival in colorectal cancer. Surgery. 2011;150(4):649–55.
Ferko A, Malý O, Örhalmi J, Dolejš J. CT/MRI pelvimetry as a useful tool when selecting patients with rectal cancer for transanal total mesorectal excision. Surg Endosc. 2016;30(3):1164–71.
Kim JY, Kim YW, Kim NK, Hur H, Lee K, Min BS, et al. Pelvic anatomy as a factor in laparoscopic rectal surgery: a prospective study. Surg Laparosc Endosc Percutan Tech. 2011;21(5):334–9.
Baek SJ, Kim CH, Cho MS, Bae SU, Hur H, Min BS, et al. Robotic surgery for rectal cancer can overcome difficulties associated with pelvic anatomy. Surg Endosc. 2015;29(6):1419–24.
Yang Y, Wang F, Zhang P, Shi C, Zou Y, Qin H. Robot-assisted versus conventional laparoscopic surgery for colorectal disease, focusing on rectal cancer: a meta-analysis. Ann Surg Oncol. 2012;19(12):3727–36.
Zur Hausen G, Gröne J, Kaufmann D, Niehues SM, Aschenbrenner K, Stroux A, et al. Influence of pelvic volume on surgical outcome after low anterior resection for rectal cancer. Int J Colorectal Dis. https://doi.org/10.1007/s00384-017-2793-9 (Epub 2017 Mar 18)
Xu W, Xu Z, Cheng H, Ying J, Cheng F, Xu W, et al. Comparison of short-term clinical outcomes between transanal and laparoscopic total mesorectal excision for the treatment of mid and low rectal cancer: a meta-analysis. 2016;42(12):1841–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Atasoy, G., Arslan, N.C., Elibol, F.D. et al. Magnetic resonance-based pelvimetry and tumor volumetry can predict surgical difficulty and oncologic outcome in locally advanced mid–low rectal cancer. Surg Today 48, 1040–1051 (2018). https://doi.org/10.1007/s00595-018-1690-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1690-3