Abstract
Purpose
Lung transplantation is accepted as an effective modality for patients with end-stage pulmonary lymphangioleiomyomatosis (LAM). Generally, bilateral lung transplantation is preferred to single lung transplantation (SLT) for LAM because of native lung-related complications, such as pneumothorax and chylothorax. It remains controversial whether SLT is a suitable surgical option for LAM. The objective of this study was to evaluate the morbidity, mortality and outcome after SLT for LAM in a lung transplant center in Japan.
Methods
We reviewed the records of 29 patients who underwent SLT for LAM in our hospital between March, 2000 and November, 2017. The data collected included the pre-transplant demographics of recipients, surgical characteristics, complications, morbidity, mortality and survival after SLT for LAM.
Results
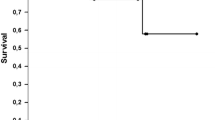
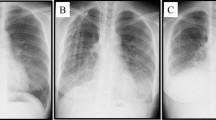
The most common complication after SLT for LAM was contralateral pneumothorax (n = 7; 24.1%). Six of these recipients were treated successfully with chest-tube placement and none required surgery for the pneumothorax. The second-most common complication was chylous pleural effusion (n = 6; 20.7%) and these recipients were all successfully treated by pleurodesis. The 5-year survival rate after SLT for LAM was 79.5%.
Conclusion
LAM-related complications after SLT for this disease can be managed. SLT is a treatment option and may improve access to lung transplantation for patients with end-stage LAM.



Similar content being viewed by others
Change history
13 June 2018
In the original publication, Fig. 3 has been incorrectly published. The correct version of Fig. 3 is given in this Correction.
References
Kpodonu J, Massad MG, Chaer RA, Caines A, Evans A, Snow NJ, et al. The US experience with lung transplantation for pulmonary lymphangioleiomyomatosis. J Hear Lung Transpl. 2005;24:1247–53.
Benden C, Rea F, Behr J, Corris PA, Reynaud-Gaubert M, Stern M, et al. Lung transplantation for lymphangioleiomyomatosis: the European experience. J Hear lung Transpl. 2009;28:1–7.
Yusen RD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Goldfarb SB, et al. The Registry of the International Society for Heart and Lung Transplantation: thirty-second Official Adult Lung and Heart-Lung Transplantation Report–2015; focus theme: early Graft Failure. J Hear Lung Transpl. 2015;34:1264–77.
Sato M, Okada Y, Oto T, Minami M, Shiraishi T, Nagayasu T, et al. Registry of the Japanese Society of Lung and Heart–Lung Transplantation: official Japanese lung transplantation report, 2014. Gen Thorac Cardiovasc Surg. 2014;62:594–601.
Pechet TT, Meyers BF, Guthrie TJ, Battafarano RJ, Trulock EP, Cooper JD, et al. Lung transplantation for lymphangioleiomyomatosis. J Heart Lung Transpl. 2004;23:301–8.
Boehler A, Speich R, Russi EW, Walter W. Lung transplantation for lymphangioleiomyomatosis. N Engl J Med. 1996;335:1275–80.
Reynaud-Gaubert M, Mornex J-F, Mal H, Treilhaud M, Dromer C, Quétant S, et al. Lung transplantation for lymphangioleiomyomatosis: the French experience. Transplantation. 2008;86:515–20.
Machuca TN, Losso MJ, Camargo SM, Schio SM, Melo IA, Hochhegger B, et al. Lung transplantation for lymphangioleiomyomatosis: single-center Brazilian experience with no chylothorax. Transpl Proc. 2011;43:236–8.
Ohara T, Oto T, Miyoshi K, Tao H, Yamane M, Toyooka S, et al. Sirolimus ameliorated post lung transplant chylothorax in lymphangioleiomyomatosis. Ann Thorac Surg. 2008;86:e7–8.
Harari S, Elia D, Torre O, Bulgheroni E, Provasi E, Moss J. Sirolimus therapy for patients with lymphangioleiomyomatosis leads to loss of chylous ascites and circulating LAM cells. Chest. 2016;150:e29–e32 (American College of Chest Physicians).
Taveira-dasilva AM, Hathaway O, Stylianou M, Moss J. Changes in lung function and chylous effusions in patients with lymphangioleiomyomatosis treated with sirolimus. Ann Intern Med. 2011;154:797–805.
Ando K, Kurihara M, Kataoka H, Ueyama M, Togo S, Sato T, et al. Efficacy and safety of low-dose sirolimus for treatment of lymphangioleiomyomatosis. Respir Investig. 2013;51:175–83.
Radzikowska E. Lymphangioleiomyomatosis: new treatment perspectives. Lung. 2015;193:467–75.
Ito T, Suno M, Sakamoto K, Yoshizaki Y, Yamamoto K, Nakanishi R, et al. Therapeutic effect of sirolimus for lymphangioleiomyomatosis remaining in the abdominopelvic region after lung transplantation: a case report. Transpl Proc. 2016;48:271–4.
King-Biggs MB, Dunitz JM, Park SJ, Kay Savik S, Hertz MI. Airway anastomotic dehiscence associated with use of sirolimus immediately after lung transplantation. Transplantation. 2003;75:1437–43.
Groetzner J, Kur F, Spelsberg F, Behr J, Frey L, Bittmann I, et al. Airway anastomosis complications in de novo lung transplantation with sirolimus-based immunosuppression. J Hear Lung Transpl. 2004;23:632–8.
Thabut G, Christie JD, Ravaud P, Castier Y, Brugière O, Fournier M, et al. Survival after bilateral versus single lung transplantation for patients with chronic obstructive pulmonary disease: a retrospective analysis of registry data. Lancet. 2008;371:744–51.
Munson JC, Christie JD, Halpern SD. The societal impact of single versus bilateral lung transplantation for chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2011;184:1282–8.
Thabut G, Christie JD, Ravaud P, Castier Y. Annals of internal medicine article survival after bilateral versus single-lung transplantation for. Ann Intern Med. 2009;151:767–74.
Ando K, Okada Y, Akiba M, Kondo T, Kawamura T, Okumura M, et al. Lung transplantation for lymphangioleiomyomatosis in Japan. PLoS One. 2016;11:1–14.
Acknowledgements
We thank Brent Bell for assistance with editing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hisashi Oishi and his co-authors have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Oishi, H., Watanabe, T., Matsuda, Y. et al. Single lung transplantation for lymphangioleiomyomatosis: a single-center experience in Japan. Surg Today 48, 944–950 (2018). https://doi.org/10.1007/s00595-018-1678-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1678-z