Abstract
Purpose
We investigated the surgical outcomes of clinical-T1b lung adenocarcinomas patients whose tumors had a solid-dominant radiological appearance and who were treated with segmentectomy or lobectomy.
Methods
We examined 154 surgically resected clinical-T1b lung adenocarcinomas with a “solid-dominant” appearance on thin-section computed tomography (CT). The preoperative thin-section CT images of all cases were reviewed. “Solid-dominant” was defined as 0.5≤ consolidation/tumor ratio (CTR) <1.0.
Results
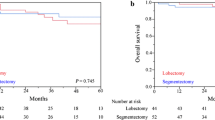
Pathological nodal metastasis, lymphatic invasion, vascular invasion, and pleural invasion were found in 7 (4.5 %), 27 (18 %), 21 (14 %), and 15 (10 %) patients with clinical-T1b solid-dominant lung adenocarcinoma, respectively. Lobectomy and segmentectomy were performed in 123 (80 %) and 31 (20 %) cases, respectively. The 3-year overall survival (OS) and relapse-free survival (RFS) of patients with clinical-T1b solid-dominant lung adenocarcinoma were 95.5 and 92.4 %, respectively. The 3-year RFS and OS did not differ significantly between the patients who underwent lobectomy or segmentectomy (3-year RFS, 92.3 vs. 93.4 %, p = 0.8713; 3-year OS, 95.3 vs. 96.6 %, p = 0.7603). Segmentectomy was not found to be a prognostic factor for RFS (p = 0.8714), or OS (p = 0.7613).
Conclusions
Segmentectomy can achieve acceptable oncological outcomes (both in terms of OS and RFS), which are similar to those achieved with standard lobectomy, in patients with clinical-T1b solid-dominant lung adenocarcinoma.




Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- GGO:
-
Ground-glass opacity
- NSCLC:
-
Non-small cell lung cancer
- PET:
-
Positron emission tomography
- SUVmax:
-
Maximum standardized uptake value
- 18F-FDG:
-
18F-fluorodeoxyglucose
- CTR:
-
Consolidation/tumor ratio
- OS:
-
Overall survival
- RFS:
-
Relapse-free survival
- CEA:
-
Carcinoembryonic antigen
References
Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409.
Suzuki K, Kusumoto M, Watanabe S, Tsuchiya R, Asamura H. Radiologic classification of small adenocarcinoma of the lung: radiologic-pathologic correlation and its prognostic impact. Ann Thorac Surg. 2006;81:413–9.
Suzuki K, Asamura H, Kusumoto M, Kondo H, Tsuchiya R. “Early” peripheral lung cancer: prognostic significance of ground glass opacity on thin-section computed tomographic scan. Ann Thorac Surg. 2002;74:1635–9.
Takamochi K, Nagai K, Yoshida J, Ohde Y, Nishimura M, Takahashi K, et al. The role of computed tomographic scanning in diagnosing mediastinal node involvement in non-small cell lung cancer. J Thorac Cardiovasc Surg. 2000;119:1135–40.
Matsunaga T, Suzuki K, Hattori A, Fukui M, Kitamura Y, Miyasaka Y, et al. Lung cancer with scattered consolidation: detection of new independent radiological category of peripheral lung cancer on thin-section computed tomography. Interact CardioVasc Thorac Surg. 2012;16:445–9.
Maeyashiki T, Suzuki K, Hattori A, Matsunaga T, Takamochi K, Oh S. The size of consolidation on thin-section computed tomography is a better predictor of survival than the maximum tumour dimension in resectable lung cancer. Eur J Cardiothorac Surg. 2012;43:915–8.
Suzuki K, Koike T, Asakawa T, Kusumoto M, Asamura H, Nagai K, et al. A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol. 2011;6:751–6.
Asamura H, Hishida T, Suzuki K, Koike T, Nakamura K, Kusumoto M, et al. Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg. 2013;146:24–30.
Keenan RJ, Landreneau RJ, Maley RH Jr, Singh D, Macherey R, Bartley S, et al. Segmental resection spares pulmonary function in patients with stage I lung cancer. Ann Thorac Surg. 2004;78:228–33 (discussion-33).
Koike T, Yamato Y, Yoshiya K, Shimoyama T, Suzuki R. Intentional limited pulmonary resection for peripheral T1 N0 M0 small-sized lung cancer. J Thorac Cardiovasc Surg. 2003;125:924–8.
Okada M, Koike T, Higashiyama M, Yamato Y, Kodama K, Tsubota N. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg. 2006;132:769–75.
Nomori H. Segmentectomy for c-T1N0M0 non-small cell lung cancer. Surg Today. 2014;44:812–9.
Aokage K, Yoshida J, Ishii G, Matsumura Y, Haruki T, Hishida T, et al. Identification of early t1b lung adenocarcinoma based on thin-section computed tomography findings. J Thorac Oncol. 2013;8:1289–94.
Hattori A, Suzuki K, Matsunaga T, Fukui M, Tsushima Y, Takamochi K, et al. Tumour standardized uptake value on positron emission tomography is a novel predictor of adenocarcinoma in situ for c-Stage IA lung cancer patients with a part-solid nodule on thin-section computed tomography scan. Interact CardioVasc Thorac Surg. 2014;18:329–34.
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, et al. Appropriate sublobar resection choice for ground glass opacity-dominant clinical stage IA lung adenocarcinoma: wedge resection or segmentectomy. Chest. 2014;145:66–71.
Hattori A, Suzuki K, Matsunaga T, Takamochi K, Oh S. Visceral pleural invasion is not a significant prognostic factor in patients with a part-solid lung cancer. Ann Thorac Surg. 2014;98:433–8.
Hattori A, Suzuki K, Takamochi K, Oh S. Clinical features of multiple lung cancers based on thin-section computed tomography: what are the appropriate surgical strategies for second lung cancers? Surg Today. 2015;45:189–96.
Hattori A, Suzuki K, Matsunaga T, Fukui M, Kitamura Y, Miyasaka Y, et al. Is limited resection appropriate for radiologically “solid” tumors in small lung cancers? Ann Thorac Surg. 2012;94:212–5.
Hattori A, Maeyashiki T, Matsunaga T, Takamochi K, Oh S, Suzuki K. Predictors of pathological non-invasive lung cancer with pure-solid appearance on computed tomography to identify possible candidates for sublobar resection. Surg Today. 2015;. doi:10.1007/s00595-015-1167-6.
Nakamura K, Saji H, Nakajima R, Okada M, Asamura H, Shibata T, et al. A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol. 2011;40:271–4.
ClinicalTrials.gov. Bethesda, MD: National Institutes of Health; Comparison of different types of surgery in treating patients with stage IA non-small cell lung cancer. Available at http://clinicaltrials.gov/ct/show/NCT00499330. Accessed 9 Jan 2012.
Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg. 1995;60:615–22 (discussion 22–23).
Rami-Porta R, Tsuboi M. Sublobar resection for lung cancer. Eur Respir J. 2009;33:426–35.
Hattori A, Suzuki K, Matsunaga T, Miyasaka Y, Takamochi K, Oh S. What is the appropriate operative strategy for radiologically solid tumours in subcentimetre lung cancer patients? Eur J Cardiothorac Surg. 2015;47:244–9.
Tsutani Y, Miyata Y, Yamanaka T, Nakayama H, Okumura S, Adachi S, et al. Solid tumors versus mixed tumors with a ground-glass opacity component in patients with clinical stage IA lung adenocarcinoma: prognostic comparison using high-resolution computed tomography findings. J Thorac Cardiovasc Surg. 2012;146:17–23.
Darling GE, Allen MS, Decker PA, Ballman K, Malthaner RA, Inculet RI, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg. 2011;141:662–70.
Acknowledgments
This work was supported in part by a Grant-in-Aid for Cancer Research from the Ministry of Health, Labour and Welfare, Japan, the Smoking Research Foundation, and the National Cancer Center Research and Development Fund (26-A-4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Rights and permissions
About this article
Cite this article
Hattori, A., Matsunaga, T., Takamochi, K. et al. The oncological outcomes of segmentectomy in clinical-T1b lung adenocarcinoma with a solid-dominant appearance on thin-section computed tomography. Surg Today 46, 914–921 (2016). https://doi.org/10.1007/s00595-015-1256-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-015-1256-6