Abstract
Purpose
Uncontrollable hepatic hydrothorax and massive ascites (H&MA) requiring preoperative drainage are sometimes encountered in liver transplantation (LT). We retrospectively analyzed the characteristics of such patients and the impact of H&MA on the postoperative course.
Methods
We evaluated 237 adult patients who underwent LT in our institute between April 2006 and October 2010.
Results
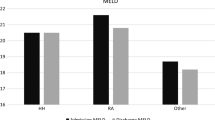
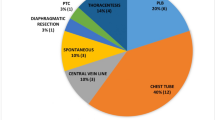
Recipients with uncontrollable H&MA (group HA: n = 36) had more intraoperative bleeding, higher Child–Pugh scores, lower serum albumin concentrations and higher blood urea nitrogen concentrations than those without uncontrollable H&MA (group C: n = 201). They were also more likely to have preoperative hepatorenal syndrome and infections. The incidence of postoperative bacteremia was higher (55.6 vs. 46.7 %, P = 0.008) and the 1- and 3-year survival rates were lower (1 year: 58.9 vs. 82.9 %; 3 years: 58.9 vs. 77.7 %; P = 0.003) in group HA than in group C. The multivariate proportional regression analyses revealed that uncontrollable H&MA and the Child–Pugh score were independent risk factors for the postoperative prognosis.
Conclusions
Postoperative infection control may be an important means of improving the outcome for patients with uncontrollable H&MA undergoing LT, and clinicians should strive to perform surgery before H&MA becomes uncontrollable.



Similar content being viewed by others
References
Taketomi A, Shirabe K, Toshima T, Hashimoto N, Kayashima H, Ikegami T, et al. The long-term outcomes of patients with hepatocellular carcinoma after living donor liver transplantation: a comparison of right and left lobe grafts. Surg Today. 2012;42:559–64.
Iida T, Kaido T, Yagi S, Yoshizawa A, Hata K, Mizumoto M, et al. Post-transplant bacteremia in adult living donor liver transplant recipients. Liver Transpl. 2010;16:1379–85.
Arroyo V, Gines P, Gerbes AL, Dudley FJ, Gentilini P, Laffi G, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. International Ascites Club. Hepatology. 1996;23:164–76.
Morrow CS, Kantor M, Armen RN. Hepatic hydrothorax. Ann Intern Med. 1958;49:193–203.
Gines P, Arroyo V. Hepatorenal syndrome. J Am Soc Nephrol. 1999;10:1833–9.
Rimola A, Garcia-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. International Ascites Club. J Hepatol. 2000;32:142–53.
Xiol X, Castellvi JM, Guardiola J, Sese E, Castellote J, Perello A, et al. Spontaneous bacterial empyema in cirrhotic patients: a prospective study. Hepatology. 1996;23:719–23.
Salerno F, Merli M, Riggio O, Cazzaniga M, Valeriano V, Pozzi M, et al. Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology. 2004;40:629–35.
Sanyal AJ, Genning C, Reddy KR, Wong F, Kowdley KV, Benner K, et al. The North American Study for the treatment of refractory ascites. Gastroenterology. 2003;124:634–41.
Hayashi PH, Forman L, Steinberg T, Bak T, Wachs M, Kugelmas M, et al. Model for end-stage liver disease score does not predict patient or graft survival in living donor liver transplant recipients. Liver Transpl. 2003;9:737–40.
Ishigami M, Honda T, Okumura A, Ishikawa T, Kobayashi M, Katano Y, et al. Use of the model for end-stage liver disease (MELD) score to predict 1-year survival of Japanese patients with cirrhosis and to determine who will benefit from living donor liver transplantation. J Gastroenterl. 2008;43:363–8.
Selzner M, Kashfi A, Cattral MS, Selzner N, McGilvray ID, Greig PD, et al. Live donor liver transplantation in high MELD score recipients. Ann Surg. 2010;251:153–7.
Somsouk M, Kornfield R, Vittinghoff E, Inadomi JM, Biggins SW. Moderate ascites identifies patients with low model for end-stage liver disease scores awaiting liver transplantation who have a high mortality risk. Liver Transpl. 2011;17:129–36.
Xiol X, Tremosa G, Castellote J, Gornals J, Lama C, Lopez C, et al. Liver transplantation in patients with hepatic hydrothorax. Transpl Int. 2005;18:672–5.
Serste T, Moreno C, Francoz C, Razek WA, Paugham C, Belghitti J, et al. The impact of preoperative hepatic hydrothorax on the outcome of adult liver transplantation. Eur J Gastroenterol Hepatol. 2010;22:207–12.
Runyon BA. Paracentesis of ascitic fluid. A safe procedure. Arch Intern Med. 1986;146:2259–61.
Runyon BA, Committee APG. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49:2087–107.
Moore KP, Aithal GP. Guidelines on the management of ascites in cirrhosis. Gut. 2006;55(Suppl 6):vi1–12.
Pozzi M, Osculati G, Boari G, Serboli P, Colombo P, Lambrughi C, et al. Time course of circulatory and humoral effects of rapid total paracentesis in cirrhotic patients with tense, refractory ascites. Gastroenterology. 1994;106:709–19.
Luca A, Feu F, Garcia-Pagan JC, Jimenez W, Arroyo V, Bosch J, et al. Favorable effects of total paracentesis on splanchnic hemodynamics in cirrhotic patients with tense ascites. Hepatology. 1994;20:30–3.
Cardenas A, Arroyo V. Management of ascites and hepatic hydrothorax. Best Pract Res Clin Gastroenterol. 2007;21:55–75.
Orman ES, Lok AS. Outcomes of patients with chest tube insertion for hepatic hydrothorax. Hepatol Int. 2009;3:582–6.
Liu LU, Haddadin HA, Bodian CA, Sigal SH, Korman JD, Bodenheimer HC Jr, et al. Outcome analysis of cirrhotic patients undergoing chest tube placement. Chest. 2004;126:142–8.
Conflict of interest
The authors have no conflicts of interest to declare in association with this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Endo, K., Iida, T., Yagi, S. et al. Impact of preoperative uncontrollable hepatic hydrothorax and massive ascites in adult liver transplantation. Surg Today 44, 2293–2299 (2014). https://doi.org/10.1007/s00595-014-0839-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-014-0839-y