Abstract
Purpose
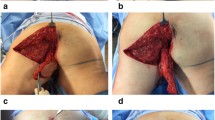
The posterior thigh flap is a reliable flap owing to the dependability of the inferior gluteal artery. Its utility for the reconstruction of sacral, perineal, ischial, pelvic, trochanteric and vulvar defects is well established. We herein describe the use of the flap for a variety of indications, and discuss the results with respect to postoperative complications in oncology patients.
Methods
We reviewed nine oncology patients who were treated with pedicled posterior thigh flaps. We assessed the use of this treatment by recording the site of the defect, the type of flap used, and the presence or absence of previous surgical procedures, radiation therapy and postoperative complications.
Results
Defects after resection of soft tissue sarcomas were the most common condition (n = 4), followed by skin cancers (n = 2), gastrointestinal cancers (n = 2) and radiation osteomyelitis (n = 1). Six patients (66 %) developed complications; three (33 %) were major and three (33 %) were minor. There was one case of total necrosis of the flap and two cases of partial necrosis.
Conclusions
In oncology patients, the posterior thigh flap is an excellent choice for the reconstruction of sacral, ischial, pelvic or buttock defects, since it does not cause any donor site morbidity.




Similar content being viewed by others
References
Hurwitz DJ. Closure of a large defect of the pelvic cavity by an extended compound myocutaneous flap based on the inferior gluteal artery. Br J Plast Surg. 1980;33:256–61.
Windhofer C, Brenner E, Moriggl B, Papp C. Relationship between the descending branch of the inferior gluteal artery and the posterior femoral cutaneous nerve applicable to flap surgery. Surg Radiol Anat. 2002;24:253–7.
Shintomi Y, Ohura T. Posterior thigh flap (in Japanese with English abstract). Keiseigeka (Jpn J PR S) 1983; 26:243–48.
Hurwitz DJ, Swartz WM, Mathes SJ. The gluteal thigh flap: a reliable, sensate flap for the closure of buttock and perineal wounds. Plast Reconstr Surg. 1981;68:521–32.
Paletta C, Bartell T, Shehadi S. Applications of the posterior thigh flap. Ann Plast Surg. 1993;30:41–7.
Rubin JA, Whetzel TP, Stevenson TR. The posterior thigh fasciocutaneous flap: vascular anatomy and clinical application. Plast Reconstr Surg. 1995;95:1228–39.
Zhang R, Sun J, Wei X, Zhang H, Liu Y, Shi M, et al. Reconstruction of defects with the posterior femoral fasciocutaneous flap after resection of malignant tumours of the femoral greater trochanter, sacrococcygeal region and knee. J Plast Reconstr Aesthet Surg. 2009;62:221–9.
Scheufler O, Farhadi J, Kovach SJ, Kukies S, Pierer G, Levin LS, et al. Anatomical basis and clinical application of the infragluteal perforator flap. Plast Reconstr Surg. 2006;118:1389–400.
Fujii M, Terashi H, Hashikawa K, Tahara S. Functional reconstruction of large anogenital defects with bilateral V-Y advancement posterior thigh fasciocutaneous flaps. J Plast Reconstr Aesthet Surg. 2007;60:1208–13.
Hurwitz DJ, Walton RL. Closure of chronic wounds of the perineal and sacral regions using the gluteal thigh flap. Ann Plast Surg. 1982;8:375–86.
Rosen JM, Mo ST, Liu A. Experience with the island inferior gluteal thigh flap compared with other local flaps for the reconstruction of the pelvic area. Ann Plast Surg. 1990;24:498–509.
Papp C, Todoroff BP, Windhofer C, Gruber S. Partial and complete reconstruction of Achilles tendon defects with the fasciocutaneous infragluteal free flap. Plast Reconstr Surg. 2003;112:777–83.
Friedman JD, Reece GR, Eldor L. The utility of the posterior thigh flap for complex pelvic and perineal reconstruction. Plast Reconstr Surg. 2010;126:146–55.
Patel AC, Kuzon WM Jr. Coverage of an ischial pressure ulcer with an interpolated contralateral posterior thigh fasciocutaneous flap. Br J Plast Surg. 2001;54:547–9.
Lin H, Hou C, Chen A, Xu Z. Long-term outcome of using posterior-thigh fasciocutaneous flaps for the treatment of ischial pressure sores. J Reconstr Microsurg. 2010;26:355–8.
Hallock GG. The random upper posterior thigh fasciocutaneous flap. Ann Plast Surg. 1994;32:367–71.
Giunta RE, Holzbach T, Taskov C, Holm PS, Brill T, Busch R, et al. Prediction of flap necrosis with laser induced indocyanine green fluorescence in a rat model. Br J Plast Surg. 2005;58:695–701.
Newman MI, Samson MC. The application of laser-assisted indocyanine green fluorescent dye angiography in microsurgical breast reconstruction. J Reconstr Microsurg. 2009;25:21–6.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saito, A., Minakawa, H., Saito, N. et al. The posterior thigh flap revisited: clinical use in oncology patients. Surg Today 44, 1013–1017 (2014). https://doi.org/10.1007/s00595-013-0635-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-013-0635-0