Abstract
Purpose
Papillary thyroid carcinoma (PTC) frequently metastasizes to and recurs in regional lymph nodes. Of the two compartments, the central compartment can be dissected through the same wound as the thyroidectomy, and the central node dissection (CND) is routinely performed in most Japanese surgical departments. However, the indications for prophylactic lateral compartment dissection (modified radical neck dissection [MND]) for low-risk PTC remain unclear. In this study, we investigated the indications for prophylactic MND for PTC patients with tumor measuring 1.1–3.0 cm without significant extrathyroid extension or distant metastasis.
Methods
We investigated the lymph node disease-free survival (LN-DFS) rates of 829 patients who underwent CND and of 414 patients who underwent MND and CND between 2005 and 2007 at Kuma Hospital.
Results
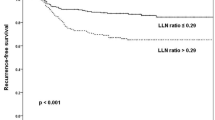
The LN-DFS of these two groups was not significantly different. In the subset of patients with CND only, clinical central node metastasis (N1a) significantly predicted a worse LN-DFS. All N1a patients recognized as showing recurrence developed such recurrence in the lateral compartment. Other conventional prognostic factors, such as sex and age, were not related to LN-DFS.
Conclusion
Taken together, N1a patients with low-risk PTC measuring 1.1–3.0 cm can be considered as candidates for prophylactic MND.
Similar content being viewed by others
References
Ruggieri M, Zullino A, Straniero A, Maiuolo A, Fumarola A, Vietri F, et al. Is minimally invasive surgery appropriate for small differentiated thyroid carcinomas? Surg Today 2010;40:418–422.
British Thyroid Association. Guidelines for the management of thyroid cancer. 2nd ed. http://www.british-thyroid-association.org/news/Docs/Thyroid_cancer_guidelines_2007.pdf.
Cooper D, Doherty G, Haugen B, Kloos R, Lee S, Mandel S, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167–1213.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Thyroid carcinoma. V. 1. http://www.nccn.org/professionals/physician_gls/PDF/thyroid/pdf
Thyroid Carcinoma Task Force. AACE/AAES medical/surgical guidelines for clinical practice: management of thyroid carcinoma. Endocr Pract 2001;7:202–220.
Japanese Society of Thyroid Surgery/Japanese Society of Endocrine Surgeons. Guidelines for management of thyroid tumor. Tokyo: Kanehara; 2010.
Ito Y, Miyauchi A, Inoue H, Fukushima M, Kihara M, Higashiyama T, et al. An observation trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg 2010;34:28–35.
Ito Y, Uruno R, Nakano K, Takamura Y, Miya A, Kobauashi K et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid 2003;13:381–388.
Ito Y, Higashiyama T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F, et al. Risk factors for recurrence to the lymph node in papillary thyroid carcinoma patients without preoperatively detectable lateral node metastasis: validity of prophylactic modified radical neck dissection. World J Surg 2007;31:2085–2091.
Antonelli A, Miccoli P, Ferdeghini M, Ferdeghini M, Di Coscio G, Alberti B, et al. Role of neck ultrasonography in the follow-up of patients operated on for thyroid cancer. Thyroid 1995;5:25–28.
Uruno T, Miyauchi A, Shimizu K, Tomoda C, Takamura Y, Ito Y, et al. Usefulness of thyroglobulin measurement in fine-needle aspiration biopsy specimens for diagnosing cervical lymph node metastasis in patients with papillary thyroid cancer. World J Surg 2005;29:483–485.
Sobin LH, Wittekind Ch (editors). UICC: TNM classification of malignant tumors. 6th ed. New York: Wiley-Liss; 2002.
Ito Y, Miyauchi A. Lateral and mediastinal lymph node dissection in differentiated thyroid carcinoma: indications, benefits, and risks. World J Surg 2007;31:905–915.
Ito Y, Miyauchi A. Prognostic factors and therapeutic strategies for differentiated carcinoma of the thyroid. Endocrine J 2009;56:177–192.
Manish D, Shah A, Hall T, Eski S. Clinical course of thyroid carcinoma after neck dissection. Laryngoscope 2003;113:2102–2107.
Balazs G, Gvory F, Lukacs G, Szakall S. Long-term follow-up of node-positive papillary thyroid carcinomas. Langenbecks Arch Surg 1998;383:180–182.
Caron N, Tan Y, Ogilvie J, Triponez F, Reiff E, Kebebew E, et al. Selective modified radical neck dissection for papillary thyroid cancer-is level I, II, and V dissection always necessary? World J Surg 2006;30:833–840.
Bhattacharyya N. Surgical treatment of cervical nodal metastasis in patients with papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 2003;129:1101–1104.
Turanili S. Is the type of dissection in lateral neck metastasis for differentiated thyroid carcinoma important? Arch Otolagyngol Head Neck Surg 2007;136:957–960.
Noguchi S, Murakami N, Yamashita H, Toda M, Kawamoto H. Papillary thyroid carcinoma: modified radical neck dissection improves prognosis. Arch Surg 1998;133:276–280.
Sato N, Oyamatsu M, Koyama Y, Emura I, Tamiya Y, Hatakeyama K. Do the level of nodal disease according to the TNM classification and the number of involved cervical nodes reflect prognosis in patients with differentiated carcinoma of the thyroid gland? J Surg Oncol 1998;69:151–155.
Sugitani I, Fumimoto Y, Yamada K, Yamamoto N. Prospective outcomes of selective lymph node dissection for papillary thyroid carcinoma based on preoperative ultrasonography. World J Surg 2008;32:2494–2502.
Simon D, Goretzki PE, Witte J. Incidence of regional recurrence guiding radicality in differentiated thyroid carcinoma. World J Surg 1996;20:860–866.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ito, Y., Tsushima, Y., Masuoka, H. et al. Significance of prophylactic modified radical neck dissection for patients with low-risk papillary thyroid carcinoma measuring 1.1–3.0 cm: First report of a trial at Kuma Hospital. Surg Today 41, 1486–1491 (2011). https://doi.org/10.1007/s00595-010-4494-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-010-4494-7