Abstract
Purpose
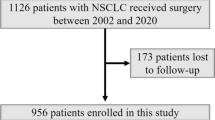
We previously demonstrated in a pilot study that postoperative cardiopulmonary complications could be reduced by selecting pulmonary resection procedures based on the results of a combination of specific preoperative cardiopulmonary function tests. The present study reports a re-examination of the criteria for preoperative screening and prospectively assessed whether the selected surgical procedures were appropriate in 200 patients who underwent the planned extent of pulmonary resection.
Methods
In 200 patients requiring lung tumor resection, five preoperative parameters (forced expiratory volume in 1 s on the intact side, maximal oxygen uptake, ejection fraction, occluded pulmonary artery pressure, and occluded total pulmonary vascular resistance index) were used to assign each patient to one of five risk categories in order to select the optimal resection procedure. Thereafter, the postoperative course was investigated to determine the value of this selection method.
Results
Thoracotomy was performed in 195 of the 200 patients (97.5%). Two patients (1%) died; one patient succumbed to acute exacerbation of interstitial pneumonia and the other patient died from pulmonary embolism. Six patients (3.1%) developed major complications after surgery and 12 patients (6.2%) had mild complications, while 175 (89.7%) showed a good postoperative course.
Conclusion
The use of five preoperative parameters to select the pulmonary resection procedure minimized postoperative death and major complications.
Similar content being viewed by others
References
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin 2007;57:43–66.
Harpole DH, DeCamp MM, Daley J, Hur K, Oprian CA, Henderson WG, et al. Prognostic models of thirty-day mortality and morbidity after major pulmonary resection. J Thorac Cardiovasc Surg 1999;117:969–979.
Rostad H, Strand TE, Naalsund A, Talleraas O, Norstein J. Lung cancer Surgery; the first 60 days. A population-based study. Eur J Cardiothorac Surg 2006;29:824–828.
Boff DJ, Allen MS, Grab JD, Gaissert HA, Harpole DH, Wright CD. Date from the society of thoracic surgeons general thoracic surgery database: The surgical management of primary lung tumors. J Thorac Cardiovasc Surg 2008;135:247–254.
Ginsberg RJ, Hill LD, Eagan RT, Thomas P, Mountain CF, Deslauriers J, et al. Modern thirty-day operative mortality for surgical resection in lung cancer. J Thorac Cardiovasc Surg 1983;86:654–658.
Wada H, Nakamura T, Nakamoto K, Maeda M, Watanabe Y. Thirty-day operative mortality for thoracotomy in lung cancer. J Thorac Cardiovasc Surg 1998;115:70–73.
Myrdal G, Gustafsson G, Lambe M, Horte LG, Stahle E. Outcome after lung cancer surgery. Factors predicting early mortality and major morbidity. Eur J Cardiothorac Surg 2001;20:694–399.
Allen MS, Darling GE, Pechet TTV, Mitchell JD, Herndon JE, Landreneau RJ, et al. Morbidity and mortality of major pulmonary resections in patients with early-stage lung cancer: Initial results of randomized, prospective ACOSOGZ0030 trial. Ann Thorac Surg 2006;81:1013–1020.
Ueda Y, Fujii Y, Udagawai H. Thoracic and cardiovascular surgery in Japan during 2006. Annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2008;56:365–388.
Nagamatsu Y, Takamori S, Hayashida R, Yamana H, Shirouzu K. Pulmonary capacity in lung cancer patients prior to lung resection. Kurume Med J 1996;43:273–277.
Nagamatsu Y, Shima I, Hayashi A, Yamana H, Shirouzu K, Ishitake T. Preoperative spirometry versus expired gas analysis during exercise testing as predictors of cardiopulmonary complications after lung resection. Surg Today 2004;34:107–110.
Nagamatsu Y, Terazaki Y, Muta F, Yamana H, Shirouzu K, Ishitake T. Expired gas analysis during exercise testing prepneumonectomy. Surg Today 2005;35:1021–1025.
Carlens E, Hanson HE, Nordenstrom B. Temporary unilateral occlusion of the pulmonary artery. J Thorac Surg 1951;22:527–536.
Sloan H, Morris JD, Figley M, Lee R. Temporary unilateral occlusion of the pulmonary artery in the preoperative evaluation of thoracic patients. J Thorac Surg 1955;30:591–597.
Nakata T, Nitta S. Research progress in the pathophysiology of the lung (in Japanese). In: Gekagaku Taikei. Tokyo: Nakayama-Shoten; 1975. p. 203–208.
Nagamatsu Y, Maeshiro K, Kashihara M, Iwasaki Y, Shima I, Yamana H, et al. Selection of pulmonary resection procedures to avoid postoperative complications. Surg Today 2007;37:202–206.
Nagamatsu Y, Maeshiro K, Kimura YN, Nishi T, Shima I, Yamana H, et al. Long term recovery of exercise capacity and pulmonary function after lobectomy. J Thorac Cardiovasc Surg 2007;134:1273–1278.
Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehab Med 1970;2:92–98.
Nagamatsu Y, Ohkita A, Kimura NY, Nakayama G, Hayashira R, Yamana H, et al. Retrospective investigation of pulmonary resection in patients with high total pulmonary vascular resistance during preoperative unilateral pulmonary artery occlusion. Gen Thorac Cardiovasc Surg 2009;57:244–249.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. GOLD scientific committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLB/WHO global initiative for chronic obstructive lung disease (GOLD) workshop summary. Am J Respir Crit Care Med 2001;163:1256–1276.
Alberg AJ, Samet JM. Epidemiology of lung cancer. Chest 2003;123(suppl):21–49.
Hanagiri T, Sugio K, Uramoto H, So T, Ichiki Y, Sugaya M, et al. Gender difference as a prognostic factor in patients undergoing resection of non-small cell lung cancer. Surg Today 2007;375:546–551.
Roselli EE, Murthy SC, Rice TW, Houghtaling PL, Pierce CD, Karchmer DP, et al. Atrial fibrillation complicating lung cancer resection. J Thorac Cardiovasc Surg 2005;130:438–444.
Weisman IM. Cardiopulmonary exercise testing in the preoperative assessment for lung resection surgery. Semin Thoracic Cardiovasc Surg 2001;13:116–125.
Beckles MA, Spiro SG, Colice GL, Rudd RM. The physiologic evaluation of patients with lung cancer being considered for resectional surgery. Chest 2003;123(suppl):105–114.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Nagamatsu, Y., Iwasaki, Y., Kashihara, M. et al. Selection of pulmonary resection procedures to reduce postoperative complications in 200 patients. Surg Today 41, 780–786 (2011). https://doi.org/10.1007/s00595-010-4350-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-010-4350-9