Abstract
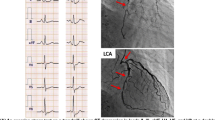
We performed successful simultaneous operations for an abdominal aortic aneurysm (AAA) and liver cancer in a patient complicated by severe ischemic heart disease. A 59-year-old man with a history of liver dysfunction presented with acute epigastric pain. Abdominal computed tomography findings of ascites and a liver tumor indicated a diagnosis of ruptured hepatocellular carcinoma. He had a concomitant 65-mm AAA and a 48-mm right common iliac aneurysm. Elective surgery was scheduled because of his good general condition. Although triple-vessel disease was detected preoperatively, there were no graftable coronary arteries. The aneurysms were repaired first to utilize intra-aortic balloon pumping (IABP) during resection of the liver cancer, followed by left lateral segmentectomy. Perioperative hemodynamics were maintained by administering catecholamines and vasodilators, without the need for IABP. The patient was discharged on the 21st postoperative day without any complications, and no recurrence of liver cancer has been found in the 5 months since his operation.
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Manabe, H., Takagi, H., Mori, Y. et al. Simultaneous Operations for Abdominal Aortic Aneurysm and Liver Cancer Complicated by Severe Ischemic Heart Disease: Report of a Case . Surg Today 33, 612–616 (2003). https://doi.org/10.1007/s00595-003-2543-1
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00595-003-2543-1