Abstract
Aims
Previous studies have shown that higher hemoglobin A1c (HbA1c) levels within the normal range during pregnancy can increase the risk of adverse birth outcomes. However, the effects of the longitudinal HbA1c trajectory during pregnancy on adverse birth outcomes among non-gestational diabetic women are poorly characterized. We aimed to identify HbA1c trajectory during pregnancy among non-gestational diabetic women and to estimate their associations with adverse birth outcomes.
Methods
Data was extracted from the Information System of Guangdong Women and Children Hospital, China, from January 2017 to July 2022. This study involved 13,979 women who did not have gestational diabetes mellitus and underwent repeated HbA1c measurements during pregnancy. Latent mixture modeling was used to identify HbA1c trajectory groups. Logistic regression was applied to explore the associations between HbA1c trajectory groups and adverse birth outcomes, including preterm delivery, low birth weight, macrosomia, small for gestational age, and large for gestational age (LGA).
Results
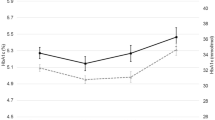
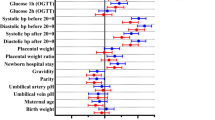
Three HbA1c trajectory groups were identified: low-stable (range 4.0% [20 mmol/mol]–4.4% [25 mmol/mol]), moderate-stable (range 4.6% [27 mmol/mol]–5.1% [32 mmol/mol]), and elevated-increasing (range 5.0% [31 mmol/mol]–5.6% [38 mmol/mol]). Compared with the low-stable HbA1c group, the elevated-increasing group had a higher risk of preterm delivery and LGA. The adjusted OR (95% CIs) were 1.67 (1.13, 2.49) and 1.47 (1.01, 2.12) for preterm delivery and LGA, respectively.
Conclusions
Among non-gestational diabetic women, the elevated-increasing HbA1c trajectory group was associated with a higher risk of preterm delivery and LGA. This finding emphasizes the importance of maintaining optimal HbA1c levels throughout pregnancy.

Similar content being viewed by others
References
Ye W, Luo C, Huang J et al (2022) Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis. BMJ 377:e67946. https://doi.org/10.1136/bmj-2021-067946
Bianco ME, Kuang A, Josefson JL et al (2021) Hyperglycemia and adverse pregnancy outcome follow-up study: newborn anthropometrics and childhood glucose metabolism. Diabetologia 64(3):561–570. https://doi.org/10.1007/s00125-020-05331-0
Farrar D, Simmonds M, Bryant M et al (2016) Hyperglycaemia and risk of adverse perinatal outcomes: systematic review and meta-analysis. BMJ 354:i4694. https://doi.org/10.1136/bmj.i4694
Li K, Li X, Morse AN et al (2022) Residual risk associations between initial hyperglycemia and adverse pregnancy outcomes in a large cohort including 6709 women with gestational diabetes. Diabetes Metab 48(1):101320. https://doi.org/10.1016/j.diabet.2022.101320
Sert UY, Ozgu-Erdinc AS (2021) Gestational diabetes mellitus screening and diagnosis. Adv Exp Med Biol 1307:231–255. https://doi.org/10.1007/5584_2020_512
Sacks DB, Arnold M, Bakris GL et al (2023) Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem 69(8):808–868. https://doi.org/10.1093/clinchem/hvad080
Jarrett RJ, Murrells TJ, Shipley MJ et al (1984) Screening blood glucose values: effects of season and time of day. Diabetologia 27(6):574–577. https://doi.org/10.1007/BF00276970
Goldstein DE (1984) Is glycosylated hemoglobin clinically useful? N Engl J Med 310(6):384–385. https://doi.org/10.1056/NEJM198402093100609
Nathan DM, Kuenen J, Borg R et al (2008) Translating the A1C assay into estimated average glucose values. Diabetes Care 31(8):1473–1478. https://doi.org/10.2337/dc08-0545
Rohlfing CL, Wiedmeyer HM, Little RR et al (2002) Defining the relationship between plasma glucose and HbA(1c): analysis of glucose profiles and HbA(1c) in the diabetes control and complications trial. Diabetes Care 25(2):275–278. https://doi.org/10.2337/diacare.25.2.275
World Health Organization (2011) Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO consultation. World Health Organization, Geneva
O’Connor C, O’Shea PM, Owens LA et al (2011) Trimester-specific reference intervals for haemoglobin A1c (HbA1c) in pregnancy. Clin Chem Lab Med 50(5):905–909. https://doi.org/10.1515/CCLM.2011.397
Mosca A, Paleari R, Dalfrà MG et al (2006) Reference intervals for hemoglobin A1c in pregnant women: data from an Italian multicenter study. Clin Chem 52(6):1138–1143. https://doi.org/10.1373/clinchem.2005.064899
Bozkurt L, Göbl CS, Leitner K et al (2020) HbA1c during early pregnancy reflects beta-cell dysfunction in women developing GDM. BMJ Open Diabetes Res Care 8(2):1. https://doi.org/10.1136/bmjdrc-2020-001751
Bi J, Ji C, Wu Y et al (2020) Association between maternal normal range HbA1c values and adverse birth outcomes. J Clin Endocrinol Metab 105(6):1. https://doi.org/10.1210/clinem/dgaa127
Carlsen EØ, Harmon Q, Magnus MC et al (2022) Glycated haemoglobin (HbA1c) in mid-pregnancy and perinatal outcomes. Int J Epidemiol 51(3):759–768. https://doi.org/10.1093/ije/dyab270
Edelson PK, James KE, Leong A et al (2020) Longitudinal changes in the relationship between hemoglobin A1c and glucose tolerance across pregnancy and postpartum. J Clin Endocrinol Metab 105(5):e1999–e2007. https://doi.org/10.1210/clinem/dgaa053
Hughes RC, Rowan J, Florkowski CM (2016) Is there a role for HbA1c in pregnancy? Curr Diab Rep 16(1):5. https://doi.org/10.1007/s11892-015-0698-y
Hughes RC, Moore MP, Gullam JE et al (2014) An early pregnancy HbA1c ≥ 5.9% (41 mmol/mol) is optimal for detecting diabetes and identifies women at increased risk of adverse pregnancy outcomes. Diabetes Care 37(11):2953–2959. https://doi.org/10.2337/dc14-1312
Lowe LP, Metzger BE, Dyer AR et al (2012) Hyperglycemia and adverse pregnancy outcome (HAPO) study: associations of maternal A1C and glucose with pregnancy outcomes. Diabetes Care 35(3):574–580. https://doi.org/10.2337/dc11-1687
Nagin DS (2014) Group-based trajectory modeling: an overview. Ann Nutr Metab 65(2–3):205–210. https://doi.org/10.1159/000360229
Metzger BE, Gabbe SG, Persson B et al (2010) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682. https://doi.org/10.2337/dc09-1848
Li MF, Ma L, Yu TP et al (2020) Adverse maternal and neonatal outcomes in pregnant women with abnormal glucose metabolism. Diabetes Res Clin Pract 161:108085. https://doi.org/10.1016/j.diabres.2020.108085
Barbry F, Lemaitre M, Ternynck C et al (2022) HbA1c at the time of testing for gestational diabetes identifies women at risk for pregnancy complications. Diabetes Metab 48(3):101313. https://doi.org/10.1016/j.diabet.2021.101313
Chehab RF, Ferrara A, Greenberg MB et al (2022) Glycemic control trajectories and risk of perinatal complications among individuals with gestational diabetes. JAMA Netw Open 5(9):e2233955. https://doi.org/10.1001/jamanetworkopen.2022.33955
Rafat D, Ahmad J (2012) HbA1c in pregnancy. Diabetes Metab Syndr 6(1):59–64. https://doi.org/10.1016/j.dsx.2012.05.010
Metzger BE, Lowe LP, Dyer AR et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358(19):1991–2002. https://doi.org/10.1056/NEJMoa0707943
Worth R, Potter JM, Drury J et al (1985) Glycosylated haemoglobin in normal pregnancy: a longitudinal study with two independent methods. Diabetologia 28(2):76–79. https://doi.org/10.1007/BF00279919
Hiramatsu Y, Shimizu I, Omori Y et al (2012) Determination of reference intervals of glycated albumin and hemoglobin A1c in healthy pregnant Japanese women and analysis of their time courses and influencing factors during pregnancy. Endocr J 59(2):145–151. https://doi.org/10.1507/endocrj.k10e-410
Sánchez-González CM, Castillo-Mora A, Alvarado-Maldonado IN et al (2018) Reference intervals for hemoglobin A1c (HbA1c) in healthy Mexican pregnant women: a cross-sectional study. BMC Pregnancy Childbirth 18(1):424. https://doi.org/10.1186/s12884-018-2057-x
Funding
This study was supported by the National Natural Science Foundation of China (82073660, 82003479) and China Postdoctoral Science Foundation (2019M662646, 2020T130220).
Author information
Authors and Affiliations
Contributions
JP and LZ conceived the study and drafted the manuscript. GJF and GCL critically reviewed the manuscript. All authors provided substantial contributions to the interpretation of data, made critical revisions to the manuscript and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was conducted following the Helsinki Declaration, and the study protocol was approved by the ethics committee of the Guangdong Women and Children Hospital (Approval Number 202201203).
Informed consent
As all data used in this study was de-identified, no written informed consent was obtained.
Additional information
Managed By Annunziata Lapolla.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peng, J., Zhang, L., Zheng, L. et al. Association between hemoglobin A1c trajectory during pregnancy and adverse birth outcomes among non-gestational diabetic women. Acta Diabetol (2024). https://doi.org/10.1007/s00592-024-02283-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00592-024-02283-4