Abstract
Aim
Women with twin pregnancies have an increased risk of gestational diabetes mellitus (GDM). Assisted reproductive technology (ART) and pre-pregnancy smoking were both associated with GDM. However, the relationships between pre-pregnancy smoking and ART and GDM in twin pregnancies were unclear. Herein, this study aims to explore the roles of pre-pregnancy smoking and ART in GDM among women with twin pregnancies.
Methods
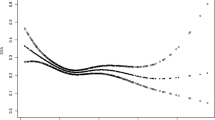
Data of women with twin pregnancies were extracted from the National Vital Statistics System (NVSS) database in 2016–2020 in this retrospective cohort study. Univariate and multivariate logistic regression analyses were used to explore the associations between pre-pregnancy smoking and ART and GDM in women with twin pregnancies. The evaluation index was odds ratios (ORs) with 95% confidence intervals (CIs). Subgroup analysis of age and BMI was also performed.
Results
A total of 19,860 (9.15%) women had GDM in our study. After adjusting for covariates, we found that receiving ART was associated with high odds of GDM [OR = 1.41, 95% CI (1.34–1.48)], while pre-pregnancy smoking combined with ART was associated with higher odds of GDM [OR = 1.66, 95% CI (1.14–2.42)]. In addition, these relationships were also found in women who aged ≥ 35 years old [OR = 1.98, 95% CI (1.14–3.44)] and with BMI ≥ 25 kg/m2 [OR = 1.69, 95% CI (1.11–2.55)].
Conclusion
Pre-pregnancy smoking may further increase the risk of GDM from ART in women with twin pregnancies. In clinical, women who are ready to receive ART treatment are recommend to quit smoking, which may reduce the risk of GDM and prevent adverse pregnancy outcomes.

Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from NVSS database, https://www.cdc.gov/nchs/nvss/index.htm.
References
Saravanan P, Diabetes in Pregnancy Working G, Maternal Medicine Clinical Study G, Royal College of O, Gynaecologists UK (2020) Gestational diabetes: opportunities for improving maternal and child health. Lancet Diabetes Endocrinol 8 (9):793-800. doi: https://doi.org/10.1016/S2213-8587(20)30161-3
Wang H, Li N, Chivese T et al (2022) IDF diabetes atlas: estimation of global and regional gestational diabetes mellitus prevalence for 2021 by international association of diabetes in pregnancy study group’s criteria. Diabetes Res Clin Pract 183:109050. https://doi.org/10.1016/j.diabres.2021.109050
Gregory ECW, Ely DM (2023) Trends and characteristics in prepregnancy diabetes: United States, 2016–2021. Natl Vital Stat Rep 72(6):1–13 (PMID: 37256333)
Moon JH, Jang HC (2022) Gestational diabetes mellitus: diagnostic approaches and maternal-offspring complications. Diabetes Metab J 46(1):3–14. https://doi.org/10.4093/dmj.2021.0335
Alkaabi J, Almazrouei R, Zoubeidi T et al (2020) Burden, associated risk factors and adverse outcomes of gestational diabetes mellitus in twin pregnancies in Al Ain. UAE BMC Pregnancy Childbirth 20(1):612. https://doi.org/10.1186/s12884-020-03289-w
Dugas C, Perron J, Kearney M et al (2017) Postnatal prevention of childhood obesity in offspring prenatally exposed to gestational diabetes mellitus: where are we now? Obes Facts 10(4):396–406. https://doi.org/10.1159/000477407
Leng J, Shao P, Zhang C et al (2015) Prevalence of gestational diabetes mellitus and its risk factors in Chinese pregnant women: a prospective population-based study in Tianjin, China. PLoS ONE 10(3):0121029. https://doi.org/10.1371/journal.pone.0121029
Barchilon-Tiosano L, Sheiner E, Wainstock T, Sergienko R, Okby-Cronin R (2021) Long-term risk for maternal cardiovascular morbidities in twin pregnancies complicated with gestational diabetes mellitus: a retrospective cohort study(dagger). J Matern Fetal Neonatal Med 34(16):2677–2681. https://doi.org/10.1080/14767058.2019.1670805
Schwartz DB, Daoud Y, Zazula P et al (1999) Gestational diabetes mellitus: metabolic and blood glucose parameters in singleton versus twin pregnancies. Am J Obstet Gynecol 181(4):912–914. https://doi.org/10.1016/s0002-9378(99)70324-8
Dimitris MC, Kaufman JS, Bodnar LM, Platt RW, Himes KP, Hutcheon JA (2022) Gestational diabetes in twin versus singleton pregnancies with normal weight or overweight pre-pregnancy body mass index: the mediating role of mid-pregnancy weight gain. Epidemiology 33(2):278–286. https://doi.org/10.1097/EDE.0000000000001454
Shiqiao H, Bei X, Yini Z, Lei J (2020) Risk factors of gestational diabetes mellitus during assisted reproductive technology procedures. Gynecol Endocrinol 36(4):318–321. https://doi.org/10.1080/09513590.2019.1648418
Fill Malfertheiner S, Gutknecht D, Bals-Pratsch M (2017) Preconception optimization of glucose and insulin metabolism in women wanting to conceive - high rate of spontaneous conception prior to planned assisted reproduction. Geburtshilfe Frauenheilkd 77(12):1312–1319. https://doi.org/10.1055/s-0043-122279
Bianchi C, Brocchi A, Baronti W et al (2023) Assisted reproductive technology, risk of gestational diabetes, and perinatal outcomes in singleton pregnancies. Diabetes Metab Res Rev 39(5):3625. https://doi.org/10.1002/dmrr.3625
Gao R, Zhao K, Zhou J et al (2022) Effects of gestational diabetes mellitus and assisted reproductive technology treatment on the risk of preterm singleton birth. Front Nutr 9:977195. https://doi.org/10.3389/fnut.2022.977195
Banker M, Dyer S, Chambers GM et al (2013) International committee for monitoring assisted reproductive technologies (ICMART): world report on assisted reproductive technologies. Fertil Steril 116(3):741–756. https://doi.org/10.1016/j.fertnstert.2021.03.039
Wen SW, Miao Q, Taljaard M et al (2020) Associations of assisted reproductive technology and twin pregnancy with risk of congenital heart defects. JAMA Pediatr 174(5):446–454. https://doi.org/10.1001/jamapediatrics.2019.6096
Allen VM, Wilson RD, Cheung A (2006) Pregnancy outcomes after assisted reproductive technology. J Obstet Gynaecol Can 28(3):220–233. https://doi.org/10.1016/S1701-2163(16)32112-0
Toner JP, Coddington CC, Doody K, et al (2016) Society for assisted reproductive technology and assisted reproductive technology in the United States: a 2016 update. Fertil Steril 106(3):541–546. https://doi.org/10.1016/j.fertnstert.2016.05.026
Wang YA, Nikravan R, Smith HC, Sullivan EA (2013) Higher prevalence of gestational diabetes mellitus following assisted reproduction technology treatment. Hum Reprod 28(9):2554–2561. https://doi.org/10.1093/humrep/det270
Kataria Y, Gaewsky L, Ellervik C (2019) Prenatal smoking exposure and cardio-metabolic risk factors in adulthood: a general population study and a meta-analysis. Int J Obes (Lond) 43(4):763–773. https://doi.org/10.1038/s41366-018-0206-y
Masalin S, Kautiainen H, Gissler M, Pennanen P, Eriksson JG, Laine MK (2020) Impact of smoking on gestational diabetes mellitus and offspring birthweight in primiparous women. Acta Obstet Gynecol Scand 99(12):1632–1639. https://doi.org/10.1111/aogs.13924
Na J, Chen H, An H et al (2022) Passive smoking and risk of gestational diabetes mellitus among nonsmoking women: a prospective cohort study in China. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph19084712
Wang JW, Cao SS, Hu RY, Wang M (2020) Association between cigarette smoking during pregnancy and gestational diabetes mellitus: a meta-analysis. J Matern Fetal Neonatal Med 33(5):758–767. https://doi.org/10.1080/14767058.2018.1500547
Hosler AS, Nayak SG, Radigan AM (2011) Stressful events, smoking exposure and other maternal risk factors associated with gestational diabetes mellitus. Paediatr Perinat Epidemiol 25(6):566–574. https://doi.org/10.1111/j.1365-3016.2011.01221.x
Haskins AE, Bertone-Johnson ER, Pekow P, Carbone E, Fortner RT, Chasan-Taber L (2010) Smoking during pregnancy and risk of abnormal glucose tolerance: a prospective cohort study. BMC Pregnancy Childbirth 10:55. https://doi.org/10.1186/1471-2393-10-55
Liu T, Gao R, Liu Y et al (2022) Hypertensive disorders of pregnancy and neonatal outcomes in twin vs. singleton pregnancies after assisted reproductive technology. Front Pediatr 10:839882. https://doi.org/10.3389/fped.2022.839882
Kim MK, Han K, You SY, Kwon HS, Yoon KH, Lee SH (2020) Prepregnancy smoking and the risk of gestational diabetes requiring insulin therapy. Sci Rep 10(1):13901. https://doi.org/10.1038/s41598-020-70873-7
Brandt JS, Cruz Ithier MA, Rosen T, Ashkinadze E (2019) Advanced paternal age, infertility, and reproductive risks: a review of the literature. Prenat Diagn 39(2):81–87. https://doi.org/10.1002/pd.5402
Dietz P, Bombard J, Mulready-Ward C et al (2015) Validation of selected items on the 2003 U.S. standard certificate of live birth: New York City and Vermont. Public Health Rep 130(1):60–70. https://doi.org/10.1177/003335491513000108
Martin JA, Hamilton BE, Osterman MJ (2012) Three decades of twin births in the United States, 1980–2009. NCHS Data Brief 80:1–8 (PMID: 22617378)
Caserta D, Bordi G, Stegagno M, Filippini F, Podagrosi M, Roselli D, Moscarini M (2014) Maternal and perinatal outcomes in spontaneous versus assisted conception twin pregnancies. Eur J Obstet Gynecol Reprod Biol 174:64–69. https://doi.org/10.1016/j.ejogrb.2013.12.011
Wang AY, Safi N, Ali F, Lui K, Li Z, Umstad MP, Sullivan EA (2018) Neonatal outcomes among twins following assisted reproductive technology: an Australian population-based retrospective cohort study. BMC Pregnancy Childbirth 18(1):320. https://doi.org/10.1186/s12884-018-1949-0
Rashid D, Alalaf S (2020) Maternal and perinatal outcomes in twin pregnancies conceived spontaneously and by assisted reproductive techniques: cross-sectional study. East Mediterr Health J 26(10):1285–1293. https://doi.org/10.26719/emhj.20.041
Maroufizadeh S, Navid B, Alizadeh A et al (2021) Risk of gestational diabetes mellitus following assisted reproductive technology: systematic review and meta-analysis of 59 cohort studies. J Matern Fetal Neonatal Med 34(16):2731–2740. https://doi.org/10.1080/14767058.2019.1670790
Sibai BM, Ross MG (2010) Hypertension in gestational diabetes mellitus: pathophysiology and long-term consequences. J Matern Fetal Neonatal Med 23(3):229–233. https://doi.org/10.3109/14767050903550899
Carson SA, Kallen AN (2021) Diagnosis and Management of Infertility: A Review. JAMA 326(1):65–76. https://doi.org/10.1001/jama.2021.4788
Hu M, Zhang Y, Guo X, Jia W, Liu G, Zhang J, Li J, Cui P, Sferruzzi-Perri AN, Han Y, Wu X, Ma H, Brannstrom M, Shao LR, Billig H (2019) Hyperandrogenism and insulin resistance induce gravid uterine defects in association with mitochondrial dysfunction and aberrant reactive oxygen species production. Am J Physiol Endocrinol Metab 316(5):E794–E809. https://doi.org/10.1152/ajpendo.00359.2018
Liu FT, Hu KL, Li R (2021) Effects of growth hormone supplementation on poor ovarian responders in assisted reproductive technology: a systematic review and meta-analysis. Reprod Sci 28(4):936–948. https://doi.org/10.1007/s43032-020-00298-0
Cui L, Lin Y, Wang F, Chen C (2021) Effectiveness of progesterone-primed ovarian stimulation in assisted reproductive technology: a systematic review and meta-analysis. Arch Gynecol Obstet 303(3):615–630. https://doi.org/10.1007/s00404-020-05939-y
Kjerulff LE, Sanchez-Ramos L, Duffy D (2011) Pregnancy outcomes in women with polycystic ovary syndrome: a metaanalysis. Am J Obstet Gynecol 204(6):551–556. https://doi.org/10.1016/j.ajog.2011.03.021
Pinborg A, Lidegaard O, Freiesleben N, Andersen AN (2007) Vanishing twins: a predictor of small-for-gestational age in IVF singletons. Hum Reprod 22(10):2707–2714. https://doi.org/10.1093/humrep/dem225
Bar-Zeev Y, Haile ZT, Chertok IA (2020) Association between prenatal smoking and gestational diabetes mellitus. Obstet Gynecol 135(1):91–99. https://doi.org/10.1097/AOG.0000000000003602
Zhang Y, Xiao CM, Zhang Y, Chen Q, Zhang XQ, Li XF, Shao RY, Gao YM (2021) Factors associated with gestational diabetes mellitus: a meta-analysis. J Diabetes Res 2021:6692695. https://doi.org/10.1155/2021/6692695
Potkonjak AM, Djakovic I, Sabolovic Rudman S, Poljak L, Kosec V (2021) Risk assessment in pregnancy among women aged over forty. Acta Clin Croat 60(2):290–295. https://doi.org/10.20471/acc.2021.60.02.16
Shan D, Qiu PY, Wu YX et al (2018) Pregnancy outcomes in women of advanced maternal age: a retrospective cohort study from China. Sci Rep 8(1):12239. https://doi.org/10.1038/s41598-018-29889-3
Li Y, Ren X, He L, Li J, Zhang S, Chen W (2020) Maternal age and the risk of gestational diabetes mellitus: a systematic review and meta-analysis of over 120 million participants. Diabetes Res Clin Pract 162:108044. https://doi.org/10.1016/j.diabres.2020.108044
Pinzauti S, Ferrata C, Vannuccini S et al (2016) Twin pregnancies after assisted reproductive technologies: the role of maternal age on pregnancy outcome. Eur J Obstet Gynecol Reprod Biol 206:198–203. https://doi.org/10.1016/j.ejogrb.2016.09.019
Laine MK, Kautiainen H, Gissler M et al (2018) Gestational diabetes in primiparous women-impact of age and adiposity: a register-based cohort study. Acta Obstet Gynecol Scand 97(2):187–194. https://doi.org/10.1111/aogs.13271
Farhi J, Ben-Haroush A, Sapir O, Fisch B, Ashkenazi J (2010) High-quality embryos retain their implantation capability in overweight women. Reprod Biomed Online 21(5):706–711. https://doi.org/10.1016/j.rbmo.2010.06.040
Sun H, Liu Y, Huang S, Liu X, Li G, Du Q (2021) Association between pre-pregnancy body mass index and maternal and neonatal outcomes of singleton pregnancies after assisted reproductive technology. Front Endocrinol (Lausanne) 12:825336. https://doi.org/10.3389/fendo.2021.825336
Luke B, Brown MB, Stern JE et al (2011) Female obesity adversely affects assisted reproductive technology (ART) pregnancy and live birth rates. Hum Reprod 26(1):245–252. https://doi.org/10.1093/humrep/deq306
Zehravi M, Maqbool M, Ara I (2021) Correlation between obesity, gestational diabetes mellitus, and pregnancy outcomes: an overview. Int J Adolesc Med Health 33(6):339–345. https://doi.org/10.1515/ijamh-2021-0058
Kim JH, Shim KW, Yoon YS, Lee SY, Kim SS, Oh SW (2012) Cigarette smoking increases abdominal and visceral obesity but not overall fatness: an observational study. PLoS ONE 7(9):e45815. https://doi.org/10.1371/journal.pone.0045815
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
LZ and YJ designed the study. LZ wrote the manuscript. YH and MZ collected, analyzed, and interpreted the data. YJ critically reviewed, edited, and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The requirement of ethical approval for this was waived by the Institutional Review Board of Nantong Maternal and Child Health Care Hospital, because the data was accessed from NVSS (a publicly available database).
Consent for publication
Not applicable.
Informed consent
The need for written informed consent was waived by the Institutional Review Board of Nantong Maternal and Child Health Care Hospital due to retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Pregnancy and Diabetes, managed by Antonio Secchi and Marina Scavini.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, L., Huang, Y., Zhang, M. et al. Synergistic effect between pre-pregnancy smoking and assisted reproductive technology on gestational diabetes mellitus in twin pregnancies. Acta Diabetol 61, 205–214 (2024). https://doi.org/10.1007/s00592-023-02183-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02183-z