Abstract
Aims
Sodium glucose transporter inhibitors (SGLT2i) therapy is associated with an increase in hematocrit as a class effect. There is a lack of information regarding the clinical magnitude and significance of hematocrit elevation, especially cardiovascular outcomes in patients with polycythemia and possible masking of lower hemoglobin levels as a sign of potential severe disease.
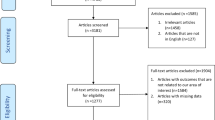
Methods
A retrospective study utilizing large community healthcare provider electronic database. Hematocrit levels and variables with potential effect on hematocrit change were compared before and during SGLT2i treatment in adults with type 2 diabetes mellitus.
Results
Study population included 9646 patients treated with Dapagliflozin or Empagliflozin between 01.2015 and 06.2019. Hematocrit levels were significantly higher after treatment initiation (2.1%), with higher median elevation among male vs female (2.3% vs. 1.8%). Anemia prevalence was significantly lower under treatment (20% vs. 31.6%). In multivariable model, gender, smoking status, SGLT2i type, pretreatment hematocrit, diabetes duration, body mass index and estimated glomerular filtration rate change significantly effected hematocrit change.
Conclusions
In the current study SGLT2i treatment was associated with significant hematocrit elevation, polycythemia and lower anemia prevalence. Further studies are needed to determine the clinical significance and approach to patients with pretreatment or on treatment polycythemia and the approach to patients with lower-normal hemoglobin levels under SGLT2i treatment.


Similar content being viewed by others
References
Yau K, Dharia A, Alrowiyti I, Cherney DZI (2022) Prescribing SGLT2 inhibitors in patients with CKD: expanding indications and practical considerations. Kidney Int Rep 7:1463–1476. https://doi.org/10.1016/j.ekir.2022.04.094
Zinman B, Lachin JM, Inzucchi SE (2016) Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med 374:1094
Neal B, Perkovic V, Mahaffey KW et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377:644–657. https://doi.org/10.1056/nejmoa1611925
Wiviott SD, Raz I, Bonaca MP et al (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380:347–357. https://doi.org/10.1056/nejmoa1812389
Heerspink HJL, Stefánsson BV, Correa-Rotter R et al (2020) Dapagliflozin in patients with chronic kidney disease. N Engl J Med 383:1436–1446. https://doi.org/10.1056/nejmoa2024816
Kimura T, Sanada J, Shimoda M et al (2018) Switching from low-dose thiazide diuretics to sodium–glucose cotransporter 2 inhibitor improves various metabolic parameters without affecting blood pressure in patients with type 2 diabetes and hypertension. J Diabetes Investig 9:875–881. https://doi.org/10.1111/jdi.12774
Van Raalte DH, Bjornstad P, Persson F et al (2019) The impact of sotagliflozin on renal function, albuminuria, blood pressure, and hematocrit in adults with type 1 diabetes. Diabetes Care 42:1921–1929. https://doi.org/10.2337/dc19-0937
Sano M, Goto S (2019) Possible mechanism of hematocrit elevation by sodium glucose cotransporter 2 inhibitors and associated beneficial renal and cardiovascular effects. Circulation 139:1985–1987. https://doi.org/10.1161/CIRCULATIONAHA.118.038881
Maruyama T, Takashima H, Oguma H et al (2019) Canagliflozin improves erythropoiesis in diabetes patients with anemia of chronic kidney disease. Diabetes Technol Ther 21:713–720. https://doi.org/10.1089/dia.2019.0212
Tian Q, Guo K, Deng J et al (2022) Effects of SGLT2 inhibitors on haematocrit and haemoglobin levels and the associated cardiorenal benefits in T2DM patients: a meta-analysis. J Cell Mol Med 26:540–547. https://doi.org/10.1111/jcmm.17115
Lambers Heerspink HJ, de Zeeuw D, Wie L et al (2013) Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab 15:853–862
Inzucchi SE, Zinman B, Fitchett D et al (2018) How does empagliflozin reduce cardiovascular mortality? Insights from a mediation analysis of the EMPA-REG OUTCOME trial. Diabetes Care 41:356–363. https://doi.org/10.2337/dc17-1096
David Mazer C, Hare GMT, Connelly PW et al (2020) Effect of empagliflozin on erythropoietin levels, iron stores, and red blood cell morphology in patients with type 2 diabetes mellitus and coronary artery disease. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.119.044235
Ghanim H, Abuaysheh S, Hejna J et al (2020) Dapagliflozin suppresses hepcidin and increases erythropoiesis. J Clin Endocrinol Metab 105:E1056–E1063. https://doi.org/10.1210/clinem/dgaa057
Packer M (2022) How can SGLT2 inhibitors stimulate erythrocytosis in patients who are iron deficient? Implications for understanding iron hemostasis in heart failure. Eur J Heart Fail. https://doi.org/10.1002/ejhf.2731
Li J, Neal B, Perkovic V et al (2020) Mediators of the effects of canagliflozin on kidney protection in patients with type 2 diabetes. Kidney Int 98:769–777. https://doi.org/10.1016/j.kint.2020.04.051
Li J, Woodward M, Perkovic V et al (2020) Mediators of the effects of canagliflozin on heart failure in patients with type 2 diabetes. JACC Heart Fail 8:57–66. https://doi.org/10.1016/j.jchf.2019.08.004
Irace C, Casciaro F, Scavelli FB et al (2018) Empagliflozin influences blood viscosity and wall shear stress in subjects with type 2 diabetes mellitus compared with incretin-based therapy. Cardiovasc Diabetol 17:1–9. https://doi.org/10.1186/s12933-018-0695-y
Packer M (2023) Mechanisms of enhanced renal and hepatic erythropoietin synthesis by sodium-glucose cotransporter 2 inhibitors. Eur Heart J. https://doi.org/10.1093/eurheartj/ehad235
Kim I-S, Lee BK, Yang P-S et al (2022) Sex-based approach for the clinical impact of polycythaemia on cardiovascular outcomes in the general population. Eur J Prev Cardiol 29:869–879. https://doi.org/10.1093/eurjpc/zwaa071
Sano M, Takei M, Shiraishi Y, Suzuki Y (2016) Increased hematocrit during sodium-glucose cotransporter 2 inhibitor therapy indicates recovery of tubulointerstitial function in diabetic kidneys. J Clin Med Res 8:844–847. https://doi.org/10.14740/jocmr2760w
Zinman B, Inzucchi SE, Lachin JM et al (2017) Empagliflozin and cerebrovascular events in patients with type 2 diabetes mellitus at high cardiovascular risk. Stroke 48:1218–1225. https://doi.org/10.1161/STROKEAHA.116.015756
Wong CKH, Lau KTK, Tang EHM et al (2022) Cardiovascular benefits of SGLT2 inhibitors in type 2 diabetes, interaction with metformin and role of erythrocytosis: a self-controlled case series study. Cardiovasc Diabetol 21:1–14. https://doi.org/10.1186/s12933-022-01520-w
Rosen B, Waitzberg R, Merkur S (2015) Israel: health system review. Health Syst Transit 17:1–212
Maccbitech Data&Disease registries. https://www.ksminnovation.com/maccabitech-data-and-disease
MacHtinger R, Fallach N, Goldstein I et al (2022) Ovarian stimulation for fertility treatments and risk of breast cancer: a matched cohort study. Hum Reprod 37:577–585. https://doi.org/10.1093/humrep/deab270
Heymann AD, Chodick G, Halkin H et al (2007) Description of a diabetes disease register extracted from a central database. Harefuah 146(15–17):79
Ayalew T (2022) Diagnostic approach to the patient with polycythemia. In: RA L (ed) Uptodate. UpToDate, Waltham
AlDallal SM, Jena N (2018) Prevalence of anemia in type 2 diabetic patients. J Hematol 7:57–61. https://doi.org/10.14740/jh411w
Weiss G, Schett G (2013) Anaemia in inflammatory rheumatic diseases. Nat Rev Rheumatol 9:205–215. https://doi.org/10.1038/nrrheum.2012.183
Li M, Cao Y, Olsson L (2021) A population-based study on time trends of hemoglobin in primary care comparing prediagnostic colorectal cancer patients versus age- and sex-matched controls. Scand J Gastroenterol 56:266–273. https://doi.org/10.1080/00365521.2021.1879245
Edgren G, Bagnardi V, Bellocco R et al (2010) Pattern of declining hemoglobin concentration before cancer diagnosis. Int J Cancer 127:1429–1436. https://doi.org/10.1002/ijc.25122
Kinar Y, Akiva P, Choman E et al (2017) Performance analysis of a machine learning flagging system used to identify a group of individuals at a high risk for colorectal cancer. PLoS ONE 12:1–8. https://doi.org/10.1371/journal.pone.0171759
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
The study was approved by MHS ethics committee.
Informed consent
As our study is based on a data registry, the need for informed consent was waived by the ethical committee.
Additional information
Managed By Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schwarz, Y., Klein, P. & Lev-Shalem, L. Masked anemia and hematocrit elevation under sodium glucose transporter inhibitors: findings from a large real-world study. Acta Diabetol 61, 99–105 (2024). https://doi.org/10.1007/s00592-023-02174-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02174-0