Abstract
Aims
To investigate the relationship between metabolic-associated fatty liver disease (MAFLD) and end-stage renal disease (ESRD) in patients with biopsy-confirmed diabetic nephropathy (DN).
Methods
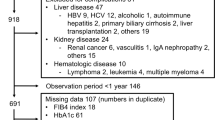
A total of 316 participants with biopsy-confirmed DN between January 2008 and December 2019 were retrospectively assessed. Kaplan–Meier curve and Cox proportional hazard models were used to compare the risk of incident ESRD in 50 patients with MAFLD and 50 patients without MAFLD, after using propensity score matching (PSM) to address the imbalances of sex, age, baseline-estimated glomerular filtration rate, serum albumin, 24-h urine protein, hemoglobin and systolic blood pressure.
Results
During the median follow-up period of 3 years, there were 19 ESRD outcome events (19%) in PSM cohort. Kaplan–Meier curve analysis suggested that renal survival significantly deteriorated in patients with MAFLD versus those without MAFLD (p = 0.021). Additionally, the hazard ratios (95% confidence interval) of MAFLD were 3.12 (1.09–8.95, p = 0.035), 3.36 (1.09–10.43, p = 0.036), 3.66 (1.22–10.98, p = 0.021), 4.25 (1.34–13.45, p = 0.014), 3.11 (1.08–8.96, p = 0.035) and 5.84 (1.94–18.5, p = 0.003) after adjustment for six models, including demographic, clinical and pathological characteristics as well as medication use at the time of renal biopsy, respectively. Besides, patients with higher liver fibrosis score had a greater possibility of ESRD, comparing to those with lower liver fibrosis score (p = 0.002).
Conclusions
MAFLD increases the risk of incident ESRD in patients with biopsy-proven DN. Further research is needed to determine whether treatment targeting MAFLD improves the prognosis of DN.



Similar content being viewed by others
Data and material availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Thomas B (2019) The global burden of diabetic kidney disease: time trends and gender gaps. Curr Diabetes Rep 19(4):18
Eslam M, Newsome PN, Sarin SK et al (2020) A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol 73(1):202–209
Anstee QM, Targher G, Day CP (2013) Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol 10(6):330–344
Wattacheril J (2020) Extrahepatic manifestations of nonalcoholic fatty liver disease. Gastroenterol Clin N Am 49(1):141–149
Sun DQ, Jin Y, Wang TY et al (2021) MAFLD and risk of CKD. Metabolism 115:154433
Sun DQ, Ye FZ, Kani HT et al (2020) Higher liver stiffness scores are associated with early kidney dysfunction in patients with histologically proven non-cirrhotic NAFLD. Diabetes Metab 46(4):288–295
Byrne CD, Targher G (2020) NAFLD as a driver of chronic kidney disease. J Hepatol 72(4):785–801
Aubert L, Sandino J, Gutierrez-Solis E et al (2022) Role of non-alcoholic fatty liver disease in the evolution of renal function in patients with diabetes mellitus. Nephrol Dial Transplant 37(6):1125–1131
Tervaert TW, Mooyaart AL, Amann K et al (2010) Pathologic classification of diabetic nephropathy. J Am Soc Nephrol 21(4):556–563
An Y, Xu F, Le W et al (2015) Renal histologic changes and the outcome in patients with diabetic nephropathy. Nephrol Dial Transplant 30(2):257–266
Eslam M, Newsome PN, Sarin SK et al (2020) A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol 73(1):202–209
Younes R, Caviglia GP, Govaere O et al (2021) Long-term outcomes and predictive ability of non-invasive scoring systems in patients with non-alcoholic fatty liver disease. J Hepatol 75(4):786–794
Zhang Z (2017) Propensity score method: a non-parametric technique to reduce model dependence. Ann Transl Med 5(1):7
Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T (2006) Variable selection for propensity score models. Am J Epidemiol 163(12):1149–1156
Zhang J, Zhang R, Wang Y et al (2019) The level of serum albumin is associated with renal prognosis in patients with Diabetic Nephropathy. J Diabetes Res 2019:7825804
Yamanouchi M, Furuichi K, Shimizu M et al (2022) Serum hemoglobin concentration and risk of renal function decline in early stages of diabetic kidney disease: a nationwide, biopsy-based cohort study. Nephrol Dial Transplant 37(3):489–497
Bakris GL, Weir MR, Shanifar S et al (2003) Effects of blood pressure level on progression of diabetic nephropathy: results from the RENAAL study. Arch Intern Med 163(13):1555–1565
Sattar N, McGuire DK, Gill JMR (2022) High circulating triglycerides are most commonly a marker of ectopic fat accumulation: connecting the clues to advance lifestyle interventions. Circulation 146(2):77–79
Catalano D, Trovato GM, Martines GF, Pirri C, Trovato FM (2011) Renal function and severity of bright liver. Relationship with insulin resistance, intrarenal resistive index, and glomerular filtration rate. Hepatol Int 5(3):822–829
de Vries AP, Ruggenenti P, Ruan XZ et al (2014) Fatty kidney: emerging role of ectopic lipid in obesity-related renal disease. Lancet Diabetes Endocrinol 2(5):417–426
Mitrofanova A, Burke G, Merscher S, Fornoni A (2021) New insights into renal lipid dysmetabolism in diabetic kidney disease. World J Diabetes 12(5):524–540
Hoffler U, Hobbie K, Wilson R et al (2009) Diet-induced obesity is associated with hyperleptinemia, hyperinsulinemia, hepatic steatosis, and glomerulopathy in C57Bl/6J mice. Endocrine 36(2):311–325
Unger RH, Zhou YT (2001) Lipotoxicity of beta-cells in obesity and in other causes of fatty acid spillover. Diabetes 50(Suppl 1):S118–S121
Nishi H, Higashihara T, Inagi R (2019) Lipotoxicity in kidney, heart, and skeletal muscle dysfunction. Nutrients 11(7)
Williamson RM, Price JF, Glancy S et al (2011) Prevalence of and risk factors for hepatic steatosis and nonalcoholic Fatty liver disease in people with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetes Care 34(5):1139–1144
Younossi ZM, Golabi P, de Avila L et al (2019) The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol 71(4):793–801
Cusi K, Sanyal AJ, Zhang S et al (2017) Non-alcoholic fatty liver disease (NAFLD) prevalence and its metabolic associations in patients with type 1 diabetes and type 2 diabetes. Diabetes Obes Metab 19(11):1630–1634
Tilg H, Moschen AR, Roden M (2017) NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol 14(1):32–42
Targher G, Bertolini L, Rodella S et al (2008) Non-alcoholic fatty liver disease is independently associated with an increased prevalence of chronic kidney disease and proliferative/laser-treated retinopathy in type 2 diabetic patients. Diabetologia 51(3):444–450
Mantovani A, Petracca G, Beatrice G et al (2022) Non-alcoholic fatty liver disease and risk of incident chronic kidney disease: an updated meta-analysis. Gut 71(1):156–162
Targher G, Byrne CD (2017) Non-alcoholic fatty liver disease: an emerging driving force in chronic kidney disease. Nat Rev Nephrol 13(5):297–310
Huh JH, Kim JY, Choi E, Kim JS, Chang Y, Sung KC (2017) The fatty liver index as a predictor of incident chronic kidney disease in a 10-year prospective cohort study. PLoS One 12(7):e0180951
Yeung MW, Wong GL, Choi KC et al (2017) Advanced liver fibrosis but not steatosis is independently associated with albuminuria in Chinese patients with type 2 diabetes. J Hepatol
Tuleta I, Frangogiannis NG (2021) Diabetic fibrosis. Biochim Biophys Acta Mol Basis Dis 1867(4):166044
Musso G, Gambino R, Tabibian JH et al (2014) Association of non-alcoholic fatty liver disease with chronic kidney disease: a systematic review and meta-analysis. PLoS Med 11(7):e1001680
Opazo-Ríos L, Mas S, Marín-Royo G et al (2020) Lipotoxicity and diabetic nephropathy: novel mechanistic insights and therapeutic opportunities. Int J Mol Sci 21(7)
Herman-Edelstein M, Scherzer P, Tobar A, Levi M, Gafter U (2014) Altered renal lipid metabolism and renal lipid accumulation in human diabetic nephropathy. J Lipid Res 55(3):561–572
Musso G, Cassader M, Cohney S et al (2016) Fatty liver and chronic kidney disease: novel mechanistic insights and therapeutic opportunities. Diabetes Care 39(10):1830–1845
Scheen AJ (2019) Beneficial effects of SGLT2 inhibitors on fatty liver in type 2 diabetes: A common comorbidity associated with severe complications. Diabetes Metab 45(3):213–223
DeFronzo RA, Reeves WB, Awad AS (2021) Pathophysiology of diabetic kidney disease: impact of SGLT2 inhibitors. Nat Rev Nephrol 17(5):319–334
Tang L, Wu Y, Tian M et al (2017) Dapagliflozin slows the progression of the renal and liver fibrosis associated with type 2 diabetes. Am J Physiol Endocrinol Metab 313(5):E563–E576
Packer M (2021) Mechanisms leading to differential hypoxia-inducible factor signaling in the diabetic kidney: modulation by SGLT2 inhibitors and hypoxia mimetics. Am J Kidney Dis 77(2):280–286
Anavi S, Hahn-Obercyger M, Madar Z, Tirosh O (2014) Mechanism for HIF-1 activation by cholesterol under normoxia: a redox signaling pathway for liver damage. Free Radic Biol Med 71:61–69
Newsome PN, Buchholtz K, Cusi K et al (2021) A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med 384(12):1113–1124
Tillman EJ, Rolph T (2019) FGF21: An emerging therapeutic target for non-alcoholic steatohepatitis and related metabolic diseases. Front Endocrinol (Lausanne) 11:601290
Weng W, Ge T, Wang Y et al (2020) Therapeutic effects of fibroblast growth factor-21 on diabetic nephropathy and the possible mechanism in type 1 diabetes mellitus mice. Diabetes Metab J 44(4):566–580
Holland JA, Martin WP, Docherty NG, le Roux CW (2019) Impact of intentional weight loss on diabetic kidney disease. Diabetes Obes Metab 21(10):2338–2341
Acknowledgements
This study was supported by the project of the National Natural Science Foundation of China (81970626). The funding source played no role in study design, data analysis, and manuscript writing or submission.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interests to disclose, and the results in this paper have not been published previously in whole or part.
Ethical approval
The study protocol was approved by the Institutional Review Board at the West China Hospital of Sichuan University [number 2013R01], and written informed consent was obtained from all participants.
Consent to participate
All patients have given informed consent.
Consent for publication
Written informed consent for publication was obtained from all participants.
Additional information
Managed by Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zou, Y., Zhao, L., Zhang, J. et al. Metabolic-associated fatty liver disease increases the risk of end-stage renal disease in patients with biopsy-confirmed diabetic nephropathy: a propensity-matched cohort study. Acta Diabetol 60, 225–233 (2023). https://doi.org/10.1007/s00592-022-01978-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-022-01978-w