Abstract
Purpose
To investigate the effect of metformin combined with anti-VEGF agents in patients with diabetic macular edema (DME).
Methods
This study was a prospective, nonrandomized case–control study. Patients were included in with a diagnosis of DME who received anti-VEGF agents injection. Basic information, medical history, best-corrected visual acuity (BCVA), central macular thickness (CMT), the number of intravitreal injections, panretinal photocoagulation (PRP), and macular grid photocoagulation treatment during the 6-month follow-up, were recorded for each patient.
Results
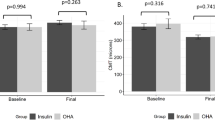
A total of 50 DME patients were collected (24 patients with a history of oral metformin ≥ 6 months and 26 patients who had not taken metformin). The BCVA and the CMT were significantly improved after anti-VEGF treatment in two groups (F1 = 19.35, F2 = 26.78; F1 = 65.45, F2 = 76.23; P < 0.05). The BCVA in the metformin group was better than that in non-metformin group at every point after treatment (F = 34.45, P < 0.05). The CMT in metformin group decreased much more than that in non-metformin group during the follow-up period (F = 87.05, P < 0.05). The injection numbers decreased in the metformin group compared with the non-metformin group (t = 5.14, P < 0.05). However, there was no difference in PRP and macular grid photocoagulation therapy between the two groups during the 6-month follow-up.
Conclusion
Metformin can enhance the therapeutic effect of anti-VEGF agents on DME patients to improve their visual acuity, improve the structure of the macular area, and reduce the number of intravitreal injections 90.



Similar content being viewed by others
Change history
03 February 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00592-022-01849-4
References
Tan GS et al (2018) Ethnic differences in the prevalence and risk factors of diabetic retinopathy: the Singapore epidemiology of eye diseases study. Ophthalmology 125(4):529–536
Yau JW et al (2012) Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 35(3):556–564
Serban R et al (2014) Visual acuity outcome in patients with diabetic maculopathy. J Med Life 7(Spec No. 2):71–5
Romero-Aroca P et al (2016) Diabetic macular edema pathophysiology: vasogenic versus inflammatory. J Diabetes Res 2016:2156273
Diabetic Retinopathy Clinical Research N et al (2015) Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med, 372(13): 1193–203
Iglicki M et al (2021) Next-generation anti-VEGF agents for diabetic macular oedema. Eye (Lond)
Iglicki M et al (2018) Progression of diabetic retinopathy severity after treatment with dexamethasone implant: a 24-month cohort study the “DR-Pro-DEX Study.” Acta Diabetol 55(6):541–547
Mello Filho P et al (2019) Effectiveness and safety of intravitreal dexamethasone implant (Ozurdex) in patients with diabetic macular edema: a real-world experience. Ophthalmologica 241(1):9–16
Zur D, Iglicki M, Loewenstein A (2019) The role of steroids in the management of diabetic macular edema. Ophthalmic Res 62(4):231–236
Holman R (2007) Metformin as first choice in oral diabetes treatment: the UKPDS experience. J Annu Diabetol Hotel Dieu, 13–20
UK Prospective Diabetes Study (UKPDS) Group (1998) Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352(9131):854–65
Evans JM et al (2006) Risk of mortality and adverse cardiovascular outcomes in type 2 diabetes: a comparison of patients treated with sulfonylureas and metformin. Diabetologia 49(5):930–936
Wurm R et al (2016) Cardiovascular safety of metformin and sulfonylureas in patients with different cardiac risk profiles. Heart 102(19):1544–1551
Fan YP et al (2020) Metformin treatment is associated with a decreased risk of nonproliferative diabetic retinopathy in patients with type 2 diabetes mellitus: a population-based cohort study. J Diabetes Res 2020:9161039
Li Y et al (2018) Association of metformin treatment with reduced severity of diabetic retinopathy in type 2 diabetic patients. J Diabetes Res 2018:2801450
Maleskic S et al (2017) Metformin use associated with protective effects for ocular complications in patients with type 2 diabetes: observational study. Acta Med Acad 46(2):116–123
Han J et al (2018) Metformin suppresses retinal angiogenesis and inflammation in vitro and in vivo. PLoS One 13(3):e0193031
Yi QY et al (2016) Metformin inhibits development of diabetic retinopathy through inducing alternative splicing of VEGF-A. Am J Transl Res 8(9):3947–3954
Zhang Y, Chen F, Wang L (2017) Metformin inhibits development of diabetic retinopathy through microRNA-497a-5p. Am J Transl Res 9(12):5558–5566
Indraccolo S et al (2015) Metformin: a modulator of bevacizumab activity in cancer? Case Rep Cancer Biol Ther 16(2):210–214
Bandello F et al (2017) Diabetic macular edema. Dev Ophthalmol 58:102–138
Brown DM et al (2015) Intravitreal aflibercept for diabetic macular edema: 100-week results from the VISTA and VIVID studies. Ophthalmology 122(10):2044–2052
Urias EA et al (2017) Novel therapeutic targets in diabetic macular edema: beyond VEGF. Vision Res 139:221–227
Adamis AP, Berman AJ (2008) Immunological mechanisms in the pathogenesis of diabetic retinopathy. Semin Immunopathol 30(2):65–84
Zhang X et al (2014) Diabetic macular edema: new concepts in patho-physiology and treatment. Cell Biosci 4:27
Nesti L, Natali A (2017) Metformin effects on the heart and the cardiovascular system: a review of experimental and clinical data. Nutr Metab Cardiovasc Dis 27(8):657–669
Graves LE, Donaghue KC (2019) Management of diabetes complications in youth. Ther Adv Endocrinol Metab 10:2042018819863226
Su YC et al (2021) Risk of diabetic macular oedema with sodium-glucose cotransporter-2 inhibitors in type 2 diabetes patients: a multi-institutional cohort study in Taiwan. Diabetes Obes Metab 23(9):2067–2076
Ishibashi R et al (2020) Safety and efficacy of ranibizumab and luseogliflozin combination therapy in patients with diabetic macular edema: protocol for a multicenter. Open-Label Randomized Controll Trial Diabetes Ther 11(8):1891–1905
Deng J et al (2018) Metformin protects against intestinal barrier dysfunction via AMPKα1-dependent inhibition of JNK signalling activation. J Cell Mol Med 22(1):546–557
Qu S et al (2020) Metformin protects ARPE-19 cells from glyoxal-induced oxidative stress. Oxid Med Cell Longev 2020:1740943
Qing L et al (2019) Metformin induces the M2 macrophage polarization to accelerate the wound healing via regulating AMPK/mTOR/NLRP3 inflammasome singling pathway. Am J Transl Res 11(2):655–668
Markowicz-Piasecka M et al (2017) Metformin: a future therapy for neurodegenerative diseases: theme: drug discovery, development and delivery in Alzheimer’s disease guest editor—Davide Brambilla. Pharm Res 34(12):2614–2627
Deng T et al (2016) Pre-stroke metformin treatment is neuroprotective involving AMPK reduction. Neurochem Res 41(10):2719–2727
Zhao M et al (2019) Neuro-protective role of metformin in patients with acute stroke and type 2 diabetes mellitus via AMPK/Mammalian target of rapamycin (mTOR) signaling pathway and oxidative stress. Med Sci Monit 25:2186–2194
张哲 et al (2018) 二甲双胍联合抗血管内皮生长因子药物治疗糖尿病视网膜病变的可能协同作用. 中华眼底病杂志, 34(05): 453–457. Zhang Z, Liu Z, Liu J, Dong L, Zhu Y, Huang L, Su R, Zhao J, Zhang X, Li X (2018) A possible synergistic effect of metformin combined with anti-vascular endothelial growth factor in the treatment of diabetic retinopathy. Chin J Fundus Dis 34(05):453–457
Batchuluun B et al (2014) Metformin and liraglutide ameliorate high glucose-induced oxidative stress via inhibition of PKC-NAD(P)H oxidase pathway in human aortic endothelial cells. Atherosclerosis 232(1):156–164
Chin JT et al (2011) A novel cardioprotective agent in cardiac transplantation: metformin activation of AMP-activated protein kinase decreases acute ischemia-reperfusion injury and chronic rejection. Yale J Biol Med 84(4):423–432
Kola M et al (2019) Repeatability and agreement of macular thickness measurements obtained with two different scan modes of the optovue rtvue optical coherence tomography device. Turk J Ophthalmol 49(2):78–83
Hodzic-Hadzibegovic D, Sander BA, Lund-Andersen H (2015) Diabetic macular oedema quantified with spectral-domain optical coherence tomography–evaluation of boundary line artefacts and the effect on retinal thickness. Acta Ophthalmol 93(1):74–82
Stattin M et al (2020) Detection rate of diabetic macular microaneurysms comparing dye-based angiography and optical coherence tomography angiography. Sci Rep 10(1):16274
Funding
Tianjin Medical University Eye Hospital clinical research fund (2016LCKY005). National Natural Science Foundation of China (NSFC) (81900891).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared that they have no conflicts of interest in this work.
Ethical approval
This study was approved by the Ethics Committee of Tianjin Medical University Eye Hospital (approval number: 2016KY-08) and adhered to the tenets of the Declaration of Helsinki. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yan Shao and Manqiao Wang are Co-first authors.
This article belongs to the topical collection Eye Complications of Diabetes, managed by Giuseppe Querques.
The original online version of this article was revised: Xiaorong Li updated as co-corresponding author.
Rights and permissions
About this article
Cite this article
Shao, Y., Wang, M., Zhu, Y. et al. Association of metformin treatment with enhanced effect of anti-VEGF agents in diabetic macular edema patients. Acta Diabetol 59, 553–559 (2022). https://doi.org/10.1007/s00592-021-01833-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-021-01833-4