Abstract
Aims
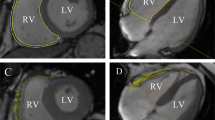
The aim of this study was to evaluate alterations in left ventricular (LV) systolic and diastolic function in subjects with prediabetes and diabetes using cardiovascular magnetic resonance-feature tracking (CMR- FT).
Methods
We included 35 subjects with prediabetes, 30 subjects with diabetes, and 33 healthy controls of similar age and sex distributions who underwent CMR examination. LV global radial, circumferential, and longitudinal strain (GRS, GCS, and GLS), peak systolic strain rate (PSSR), and peak diastolic strain rate (PDSR) were measured and compared among the three groups. Pearson’s correlation and linear regression analyses were applied for statistical analyses.
Results
Subjects with prediabetes and diabetes had a significantly lower GLS than healthy controls, but there were no significant differences in ejection fraction (EF), GRS, GCS, or global radial, circumferential and longitudinal PSSR among the three groups. Global radial, circumferential, and longitudinal PDSR in patients with diabetes were all significantly lower than those in the healthy controls. Compared to subjects with prediabetes, patients with diabetes had a significantly lower global circumferential PDSR. Global longitudinal PDSR in subjects with prediabetes was significantly lower than that in healthy controls. Multivariable linear regression analyses demonstrated that elevated HbA1c levels were independently associated with decreased global circumferential and longitudinal PDSR (β = −0.203, p = 0.023; β = −0.207, p = 0.040, respectively).
Conclusions
CMR-FT has potential value to evaluate early alterations in LV systolic and diastolic function in subjects with prediabetes and diabetes. Elevated HbA1c levels were independently associated with impaired LV diastolic function in the general population free of overt cardiovascular diseases.

Similar content being viewed by others
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cho NH, Shaw JE, Karuranga S et al (2018) IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 138:271–281. https://doi.org/10.1016/j.diabres.2018.02.023
Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H (2001) Mortality and causes of death in the WHO multinational study of vascular disease in diabetes. Diabetologia 44(Suppl 2):S14-21. https://doi.org/10.1007/pl00002934
Huang Y, Cai X, Mai W, Li M, Hu Y (2016) Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ 355:i5953. https://doi.org/10.1136/bmj.i5953
Sardu C, Trotta MC, Pieretti G et al (2021) MicroRNAs modulation and clinical outcomes at 1 year of follow-up in obese patients with pre-diabetes treated with metformin vs. placebo. Acta Diabetol 58:1381–1393. https://doi.org/10.1007/s00592-021-01743-5
D’Onofrio N, Pieretti G, Ciccarelli F et al (2019) Abdominal fat sirt6 expression and its relationship with inflammatory and metabolic pathways in pre-diabetic overweight patients. Int J Mol Sci 20:1153. https://doi.org/10.3390/ijms20051153
American Diabetes A (2020) 3. Prevention or delay of Type 2 diabetes: standards of medical care in diabetes-2020. Diabetes Care 43:S32–S36. https://doi.org/10.2337/dc20-S003
American Diabetes A (2020) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 43:S14–S31. https://doi.org/10.2337/dc20-S002
Selvin E, Lazo M, Chen Y et al (2014) Diabetes mellitus, prediabetes, and incidence of subclinical myocardial damage. Circulation 130:1374–1382. https://doi.org/10.1161/CIRCULATIONAHA.114.010815
Lin JL, Sung KT, Su CH et al (2018). Cardiac structural remodeling, longitudinal systolic strain, and torsional mechanics in lean and nonlean dysglycemic chinese adults. Circulation: Cardiovascular Imaging 11: e007047. https://doi.org/10.1161/CIRCIMAGING.117.007047
De Marco M, de Simone G, Roman MJ et al (2011) Cardiac geometry and function in diabetic or prediabetic adolescents and young adults: the strong heart study. Diabetes Care 34:2300–2305. https://doi.org/10.2337/dc11-0191
Schneider ALC, Kalyani RR, Golden S et al (2016) Diabetes and prediabetes and risk of hospitalization: the atherosclerosis risk in communities (aric) study. Diabetes Care 39:772–779. https://doi.org/10.2337/dc15-1335
Shenoy C, Romano S, Hughes A et al. (2020). Cardiac magnetic resonance feature tracking global longitudinal strain and prognosis after heart transplantation. JACC: Cardiovasc Imaging, 13:1934–1942.
Maceira AM, Guardiola S, Ripoll C, Cosin-Sales J, Belloch V, Salazar J (2020) Detection of subclinical myocardial dysfunction in cocaine addicts with feature tracking cardiovascular magnetic resonance. J Cardiovasc Magn Reson 22:70. https://doi.org/10.1186/s12968-020-00663-7
Pedrizzetti G, Claus P, Kilner PJ, Nagel E (2016) Principles of cardiovascular magnetic resonance feature tracking and echocardiographic speckle tracking for informed clinical use. J Cardiovasc Magn Reson 18:51. https://doi.org/10.1186/s12968-016-0269-7
Halliday BP, Senior R, Pennell DJ (2021) Assessing left ventricular systolic function: from ejection fraction to strain analysis. Eur Heart J 42:789–797. https://doi.org/10.1093/eurheartj/ehaa587
Jiang L, Wang J, Liu X et al (2020) The combined effects of cardiac geometry, microcirculation, and tissue characteristics on cardiac systolic and diastolic function in subclinical diabetes mellitus-related cardiomyopathy. Int J Cardiol 320:112–118. https://doi.org/10.1016/j.ijcard.2020.07.013
Liu X, Yang ZG, Gao Y et al (2018) Left ventricular subclinical myocardial dysfunction in uncomplicated type 2 diabetes mellitus is associated with impaired myocardial perfusion: a contrast-enhanced cardiovascular magnetic resonance study. Cardiovasc Diabetol 17:139. https://doi.org/10.1186/s12933-018-0782-0
Salton CJ, Chuang ML, O’Donnell CJ et al (2002) Gender differences and normal left ventricular anatomy in an adult population free of hypertension. A cardiovascular magnetic resonance study of the framingham heart study offspring cohort. J Am Coll Cardiol 39:1055–1060. https://doi.org/10.1016/s0735-1097(02)01712-6
Zhang Z, Ma Q, Cao L et al (2019) Correlation between left ventricular myocardial strain and left ventricular geometry in healthy adults: a cardiovascular magnetic resonance-feature tracking study. Int J Cardiovasc Imaging 35:2057–2065. https://doi.org/10.1007/s10554-019-01644-3
Shao G, Cao Y, Cui Y et al (2020) Early detection of left atrial and bi-ventricular myocardial strain abnormalities by MRI feature tracking in normotensive or hypertensive T2DM patients with preserved LV function. BMC Cardiovasc Disord 20:196. https://doi.org/10.1186/s12872-020-01469-2
Tadic M, Ilic S, Cuspidi C et al (2015) Left ventricular mechanics in untreated normotensive patients with type 2 diabetes mellitus: a two- and three-dimensional speckle tracking study. Echocardiography 32:947–955. https://doi.org/10.1111/echo.12790
Ernande L, Thibault H, Bergerot C et al (2012) Systolic myocardial dysfunction in patients with type 2 diabetes mellitus: identification at MR imaging with cine displacement encoding with stimulated echoes. Radiology 265:402–409. https://doi.org/10.1148/radiol.12112571
Claus P, Omar AMS, Pedrizzetti G, Sengupta PP, Nagel E (2015). Tissue tracking technology for assessing cardiac mechanics, JACC: Cardiovasc Imaging 8: 1444–1460. https://doi.org/10.1016/j.jcmg.2015.11.001
Huang D, Refaat M, Mohammedi K, Jayyousi A, Al Suwaidi J, Abi Khalil C (2017) Macrovascular complications in patients with diabetes and prediabetes. Biomed Res Int 2017:1–9. https://doi.org/10.1155/2017/7839101
Low Wang CC, Hess CN, Hiatt WR, Goldfine AB (2016) Clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus–mechanisms, management, and clinical considerations. Circulation 133:2459–2502. https://doi.org/10.1161/CIRCULATIONAHA.116.022194
Li ZL, He S, Xia CC et al (2021) Global longitudinal diastolic strain rate as a novel marker for predicting adverse outcomes in hypertrophic cardiomyopathy by cardiac magnetic resonance tissue tracking. Clin Radiol 76:78.e19-78.e25. https://doi.org/10.1016/j.crad.2020.08.019
Zhu J, Shi F, You T, Tang C, Chen J (2020) Global diastolic strain rate for the assessment of left ventricular diastolic dysfunction in young peritoneal dialysis patients: a case control study. BMC Nephrol 21:89. https://doi.org/10.1186/s12882-020-01742-8
Grigorescu ED, Lacatusu CM, Floria M, Mihai BM, Cretu I, Sorodoc L (2019) Left ventricular diastolic dysfunction in type 2 diabetes-progress and perspectives. Diagn (Basel) 9:121. https://doi.org/10.3390/diagnostics9030121
Di Pino A, Mangiafico S, Urbano F et al (2017) HbA1c identifies subjects with prediabetes and subclinical left ventricular diastolic dysfunction. J Clin Endocrinol Metab 102:3756–3764. https://doi.org/10.1210/jc.2017-00954
Tadic M, Suzic-Lazic J, Vukomanovic V, Cuspidi C, Ilic S, Celic V (2020) Functional capacity and left ventricular diastolic function in patients with type 2 diabetes. Acta Diabetol 58:107–113. https://doi.org/10.1007/s00592-020-01600-x
Ng AC, Delgado V, Bertini M et al (2009) Findings from left ventricular strain and strain rate imaging in asymptomatic patients with type 2 diabetes mellitus. Am J Cardiol 104:1398–1401. https://doi.org/10.1016/j.amjcard.2009.06.063
Sardu C, Modugno P, Castellano G et al (2021) Atherosclerotic plaque fissuration and clinical outcomes in pre-diabetics vs. normoglycemics patients affected by asymptomatic significant carotid artery stenosis at 2 years of follow-up: role of micrornas modulation: the atimir study. Biomedicines 9:401. https://doi.org/10.3390/biomedicines9040401
Sardu C, Paolisso P, Sacra C et al (2019) Effects of metformin therapy on coronary endothelial dysfunction in patients with prediabetes with stable angina and nonobstructive coronary artery stenosis: the CODYCE Multicenter prospective study. Diabetes Care 42:1946–1955. https://doi.org/10.2337/dc18-2356
Sardu C, D’Onofrio N, Torella M et al (2021) Metformin therapy effects on the expression of sodium-glucose cotransporter 2, leptin, and sirt6 levels in pericoronary fat excised from pre-diabetic patients with acute myocardial infarction. Biomedicines 9:904. https://doi.org/10.3390/biomedicines9080904
Sardu C, D’Onofrio N, Torella M et al (2019) Pericoronary fat inflammation and major adverse cardiac events (MACE) in prediabetic patients with acute myocardial infarction: effects of metformin. Cardiovasc Diabetol 18:126. https://doi.org/10.1186/s12933-019-0931-0
Tseng E, Yeh HC, Maruthur NM (2017) Metformin use in prediabetes among U.S. adults, 2005–2012. Diabetes Care 40:887–893. https://doi.org/10.2337/dc16-1509
Acknowledgements
The authors thank all the staff of Zhouxin Medical Imaging and Health Screening Center, Xiamen, China for their help in obtaining images and data.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Chinese Ethics Committee approved this study with a waiver of written informed consent (ChiECRCT20190198). Project start date: October 10, 2019.
Informed consent
Informed consent was not required for this study.
Consent to participate
All participants in this study gave written consent for participation.
Consent for publication
All participants in this study gave written consent for publication.
Additional information
Managed by Massimo Federici .
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The study was retrospectively registered and approved by the Chinese Ethics Committee (ChiECRCT20190198). Project start date: October 10, 2019.
Rights and permissions
About this article
Cite this article
Zhou, S., Zhang, Z., Zhang, Z. et al. Evaluation of left ventricular systolic and diastolic function in subjects with prediabetes and diabetes using cardiovascular magnetic resonance-feature tracking. Acta Diabetol 59, 491–499 (2022). https://doi.org/10.1007/s00592-021-01822-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-021-01822-7