Abstract
Objective
The aim of this study was to investigate the association between a relatively high HbA1c level within the normal range and the risk of adverse pregnancy outcomes.
Methods
This retrospective cohort study was conducted between March 2018 and March 2019 at Women’s Hospital, School of Medicine, Zhejiang University. Multiple logistic regression models after adjusting for plausible confounders were implemented to assess the relationships between the level of HbA1c and adverse pregnancy outcomes.
Results
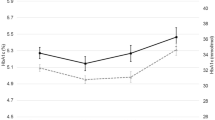
A total of 8585 women were included in our study. The rates of preterm birth, macrosomia and preeclampsia were 4.4% (380/8585), 5.3% (457/8585) and 1.7% (149/8585), respectively. After adjusting for potential confounding variables, an HbA1c range of 5.5–5.9% (37–41 mmol/mol) remained significantly associated with an increased risk of preterm delivery (a-OR 2.27; 95% CI, 1.50–3.43), macrosomia (a-OR 1.97; 95% CI, 1.32–2.94) and preeclampsia (a-OR 3.70; 95% CI, 2.07–6.60). GDM-negative pregnant women with an HbA1c level in the range of 5.5–5.9% (37–41 mmol/mol) had an increased risk of preterm delivery (a-OR 2.84; 95% CI, 1.71–4.71) and preeclampsia (a-OR 3.82; 95% CI, 1.81–8.04). However, GDM-positive pregnant women had an increased risk of macrosomia (a-OR 2.12; 95% CI, 1.13–3.97) and preeclampsia (a-OR 2.62; 95% CI, 1.01–6.81).
Conclusion
A higher HbA1c level within the normal range is an independent risk factor for preterm delivery and preeclampsia, especially among GDM-negative women. Therefore, relevant medical staff should enhance the awareness of risk and prevention to strengthen pregnancy monitoring.



Similar content being viewed by others
References
Johns EC, Denison FC, Norman JE, Reynolds RM (2018) Gestational diabetes mellitus: mechanisms, treatment, and complications. Trends Endocrinol Metab 29(11):743–754. https://doi.org/10.1016/j.tem.2018.09.004
Pintaudi B, Fresa R, Dalfra M, Dodesini AR, Vitacolonna E, Tumminia A, Sciacca L, Lencioni C, Marcone T, Lucisano G, Nicolucci A, Bonomo M, Napoli A (2018) The risk stratification of adverse neonatal outcomes in women with gestational diabetes (STRONG) study. Acta Diabetol 55(12):1261–1273. https://doi.org/10.1007/s00592-018-1208-x
Benhalima K, De Landtsheer A, Van Crombrugge P, Moyson C, Verhaeghe J, Verlaenen H, Vercammen C, Maes T, Dufraimont E, De Block C, Jacquemyn Y, Laenen A, Devlieger R, Minschart C, Mathieu C (2020) Predictors of neonatal adiposity and associations by fetal sex in women with gestational diabetes mellitus and normal glucose-tolerant women. Acta Diabetol. https://doi.org/10.1007/s00592-020-01619-0
Mckenzie-Sampson S, Paradis G, Healy-Profitos J, St-Pierre F, Auger N (2018) Gestational diabetes and risk of cardiovascular disease up to 25 years after pregnancy: a retrospective cohort study. Acta Diabetol 55(4):315–322. https://doi.org/10.1007/s00592-017-1099-2
Crowther CA, Hiller JE, Moss JR, Mcphee AJ, Jeffries WS, Robinson JS (2005) Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 352(24):2477–2486. https://doi.org/10.1056/NEJMoa042973
Association AD (2017) 2. Classification and diagnosis of diabetes. Diabetes Care 40(Suppl 1):S11-S24. https://doi.org/10.2337/dc17-S005
Yan J, Yang H (2014) Gestational diabetes in China: challenges and coping strategies. Lancet Diabetes Endocrinol 2(12):930–931. https://doi.org/10.1016/S2213-8587(14)70154-8
Li HT, Xue M, Hellerstein S, Cai Y, Gao Y, Zhang Y, Qiao J, Blustein J, Liu JM (2019) Association of China’s universal two child policy with changes in births and birth related health factors: national, descriptive comparative study. BMJ 366:l4680. https://doi.org/10.1136/bmj.l4680
Nankervis A, Mcintyre HD, Moses RG, Ross GP, Callaway LK (2013) Testing for gestational diabetes mellitus in Australia. Diabetes Care 36(5):e64. https://doi.org/10.2337/dc12-2345
Sesmilo G, Prats P, Garcia S, Rodriguez I, Rodriguez-Melcon A, Berges I, Serra B (2020) First-trimester fasting glycemia as a predictor of gestational diabetes (GDM) and adverse pregnancy outcomes. Acta Diabetol 57(6):697–703. https://doi.org/10.1007/s00592-019-01474-8
Hughes RC, Rowan J, Florkowski CM (2016) Is There a Role for HbA1c in pregnancy? Curr Diab Rep 16(1):5. https://doi.org/10.1007/s11892-015-0698-y
Association AD (2020) 14. Management of diabetes in pregnancy: standards of medical care in diabetes-2020. Diabetes Care 43(Suppl 1):S183-S192. https://doi.org/10.2337/dc20-S014
Nielsen LR, Ekbom P, Damm P, Glumer C, Frandsen MM, Jensen DM, Mathiesen ER (2004) HbA1c levels are significantly lower in early and late pregnancy. Diabetes Care 27(5):1200–1201. https://doi.org/10.2337/diacare.27.5.1200
Rowan JA, Budden A, Ivanova V, Hughes RC, Sadler LC (2016) Women with an HbA1c of 41–49 mmol/mol (5.9–6.6%): a higher risk subgroup that may benefit from early pregnancy intervention. Diabet Med 33(1):25–31. https://doi.org/10.1111/dme.12812
Hughes RC, Moore MP, Gullam JE, Mohamed K, Rowan J (2014) An early pregnancy HbA1c >/=5.9% (41 mmol/mol) is optimal for detecting diabetes and identifies women at increased risk of adverse pregnancy outcomes. Diabetes Care 37(11):2953–2959. https://doi.org/10.2337/dc14-1312
Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, Dyer AR, Leiva A, Hod M, Kitzmiler JL, Lowe LP, Mcintyre HD, Oats JJ, Omori Y, Schmidt MI (2010) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682. https://doi.org/10.2337/dc09-1848
Lowe LP, Metzger BE, Dyer AR, Lowe J, Mccance DR, Lappin TR, Trimble ER, Coustan DR, Hadden DR, Hod M, Oats JJ, Persson B (2012) Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study: associations of maternal A1C and glucose with pregnancy outcomes. Diabetes Care 35(3):574–580. https://doi.org/10.2337/dc11-1687
Huang Y, Zhang W, Go K, Tsuchiya KJ, Hu J, Skupski DW, Sie SY, Nomura Y (2020) Altered growth trajectory in children born to mothers with gestational diabetes mellitus and preeclampsia. Arch Gynecol Obstet 301(1):151–159. https://doi.org/10.1007/s00404-020-05436-2
Sun D, Mcleod A, Gandhi S, Malinowski AK, Shehata N (2017) Anemia in Pregnancy: A Pragmatic Approach. Obstet Gynecol Surv 72(12):730–737. https://doi.org/10.1097/OGX.0000000000000510
Hanas R, John G (2010) 2010 consensus statement on the worldwide standardization of the hemoglobin A1C measurement. Diabetes Care 33(8):1903–1904. https://doi.org/10.2337/dc10-0953
Mane L, Flores-Le RJ, Benaiges D, Rodriguez M, Marcelo I, Chillaron JJ, Pedro-Botet J, Llaurado G, Gortazar L, Carreras R, Paya A (2017) Role of first-trimester HbA1c as a predictor of adverse obstetric outcomes in a multiethnic cohort. J Clin Endocrinol Metab 102(2):390–397. https://doi.org/10.1210/jc.2016-2581
Holmes VA, Young IS, Patterson CC, Pearson DW, Walker JD, Maresh MJ, Mccance DR (2011) Optimal glycemic control, pre-eclampsia, and gestational hypertension in women with type 1 diabetes in the diabetes and pre-eclampsia intervention trial. Diabetes Care 34(8):1683–1688. https://doi.org/10.2337/dc11-0244
Barrett HL, Dekker NM, Jones L, O’Rourke P, Lust K, Gatford KL, De Blasio MJ, Coat S, Owens JA, Hague WM, Mcintyre HD, Callaway L, Rowan J (2013) Determinants of maternal triglycerides in women with gestational diabetes mellitus in the metformin in gestational diabetes (MiG) study. Diabetes Care 36(7):1941–1946. https://doi.org/10.2337/dc12-2132
Vambergue A, Fajardy I (2011) Consequences of gestational and pregestational diabetes on placental function and birth weight. World J Diabetes 2(11):196–203. https://doi.org/10.4239/wjd.v2.i11.196
Scavini M, Secchi A (2019) Diabetes in pregnancy. Acta Diabetol 56(7):719–721. https://doi.org/10.1007/s00592-019-01364-z
Amylidi S, Mosimann B, Stettler C, Fiedler GM, Surbek D, Raio L (2016) First-trimester glycosylated hemoglobin in women at high risk for gestational diabetes. Acta Obstet Gynecol Scand 95(1):93–97. https://doi.org/10.1111/aogs.12784
Binbir B, Yeniel AO, Ergenoglu AM, Kazandi M, Akercan F, Sagol S (2012) The role of umbilical cord thickness and HbA1c levels for the prediction of fetal macrosomia in patients with gestational diabetes mellitus. Arch Gynecol Obstet 285(3):635–639. https://doi.org/10.1007/s00404-011-1961-3
Rowan JA, Budden A, Sadler LC (2014) Women with a nondiagnostic 75 g glucose tolerance test but elevated HbA1c in pregnancy: an additional group of women with gestational diabetes. Aust N Z J Obstet Gynaecol 54(2):177–180. https://doi.org/10.1111/ajo.12166
Bonongwe P, Lindow SW, Coetzee EJ (2015) Reproducibility of a 75G oral glucose tolerance test in pregnant women. J Perinat Med 43(3):333–338. https://doi.org/10.1515/jpm-2014-0208
Funding
This work was supported by the National Key R&D Program of China (grant number: 2018YFC1002702).
Author information
Authors and Affiliations
Contributions
BBY and LWH were involved in conceptualization, investigation, data collection and analysis, and manuscript writing. XJM, KQW and LZ were involved in data collection and analysis and manuscript writing. YNZ and BZ were involved in conceptualization, investigation, funding acquisition, supervision, validation and manuscript editing.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Ethical approval
This study was approved by the Medical Ethics Committee of Women’s Hospital, School of Medicine, Zhejiang University, Hangzhou, China (Approval number: IRB-20200037-R). Since this is a retrospectively observational study with no intervention, the Ethics Committee of Women's Hospital Affiliated to Zhejiang University School of Medicine has determined exemption for informed consent of the study participants.
Informed consent
Not applicable for this study.
Additional information
This article belongs to the topical collection Pregnancy and Diabetes, managed by Antonio Secchi and Marina Scavini
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yin, B., Hu, L., Meng, X. et al. Association of higher HbA1c within the normal range with adverse pregnancy outcomes: a cross-sectional study. Acta Diabetol 58, 1081–1089 (2021). https://doi.org/10.1007/s00592-021-01691-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-021-01691-0