Abstract
Aims
To explore the association between physical activity in early pregnancy and development of preeclampsia in women with preexisting diabetes.
Methods
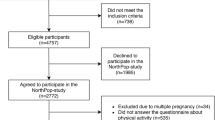
In a prospective cohort study of 189 women with preexisting diabetes (110 type 1 and 79 type 2 diabetes), physical activity during pregnancy including sedentary behavior was evaluated with the Pregnancy Physical Activity Questionnaire. Primary outcome was preeclampsia. Secondary outcomes were preterm delivery, large and small for gestational age infants.
Results
Women developing preeclampsia (n = 23) had higher diastolic blood pressure in early pregnancy (mean 82 ± 9 SD vs. 77 ± 8, p = 0.004) and were more often nulliparous (91 vs. 52%, p < 0.001) compared with the remaining women (n = 166). Total physical activity in early pregnancy was similar between the groups (median 148 metabolic equivalent of task hours per week (MET-h/week) (interquartile range 118–227) versus 153 (121–205), p = 0.97). In early pregnancy, women developing preeclampsia reported a higher level of sedentary behavior (15 MET-h/week (7–18) versus 7 (4–15); p = 0.04); however, when adjusting for parity, diastolic blood pressure and smoking, the association attenuated (p = 0.13). Total physical activity and sedentary behavior in early pregnancy were not associated with preterm delivery, large or small for gestational age infants.
Conclusions
Among women with diabetes, sedentary behavior was reported higher in early pregnancy in women developing preeclampsia compared with the remaining women, while total physical activity was similar. Sedentary behavior was a predictor of preeclampsia in the univariate analysis, but not in the multiple regression analysis, and larger studies are needed to evaluate this possible modifiable risk factor.
Trial registration The study was registered at ClinicalTrials.gov (ID: NCT02890836).

Similar content being viewed by others
References
Mol BWJ, Roberts CT, Thangaratinam S, Magee LA, de Groot CJM, Hofmeyr GJ (2016) Pre-eclampsia. Lancet 387:999–1011. https://doi.org/10.1016/S0140-6736(15)00070-7
Weissgerber TL, Mudd LM (2015) Preeclampsia and diabetes. Curr Diab Rep 15:9. https://doi.org/10.1007/s11892-015-0579-4
Aune D, Saugstad OD, Henriksen T, Tonstad S (2014) Physical activity and the risk of preeclampsia: a systematic review and meta-analysis. Epidemiology 25:331–343. https://doi.org/10.1097/EDE.0000000000000036
Wolf HT, Owe KM, Juhl M, Hegaard HK (2014) Leisure time physical activity and the risk of pre-eclampsia: a systematic review. Matern Child Heal J 18:899–910. https://doi.org/10.1007/s10995-013-1316-8
Hegaard HK, Pedersen BK, Nielsen BB, Damm P (2007) Leisure time physical activity during pregnancy and impact on gestational diabetes mellitus, pre-eclampsia, preterm delivery and birth weight: a review. Acta Obs Gynecol Scand 86:1290–1296. https://doi.org/10.1080/00016340701647341
Kasawara KT, do Nascimento SL, Costa ML, Surita FG, e Silva JL (2012) Exercise and physical activity in the prevention of pre-eclampsia: systematic review. Acta Obs Gynecol Scand 91:1147–1157. https://doi.org/10.1111/j.1600-0412.2012.01483.x
Davenport MH, Ruchat S-M, Poitras VJ et al (2018) Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Br J Sports Med 52:1367–1375. https://doi.org/10.1136/bjsports-2018-099355
Rogozinska E, Marlin N, Jackson L et al (2017) Effects of antenatal diet and physical activity on maternal and fetal outcomes: individual patient data meta-analysis and health economic evaluation. Heal Technol Assess 21:1–158. https://doi.org/10.3310/hta21410
Magro-Malosso ER, Saccone G, Di Tommaso M, Roman A, Berghella V (2017) Exercise during pregnancy and risk of gestational hypertensive disorders: a systematic review and meta-analysis. Acta Obs Gynecol Scand 96:921–931. https://doi.org/10.1111/aogs.13151
Muktabhant B, Lawrie TA, Lumbiganon P, Laopaiboon M (2015) Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd007145.pub3
da Silva SG, Ricardo LI, Evenson KR, Hallal PC (2017) Leisure-time physical activity in pregnancy and maternal-child health: a systematic review and meta-analysis of randomized controlled trials and cohort studies. Sports Med 47:295–317. https://doi.org/10.1007/s40279-016-0565-2
Clausen P, Ekbom P, Damm P et al (2007) Signs of maternal vascular dysfunction precede preeclampsia in women with type 1 diabetes. J Diabetes Complicat 21:288–293. https://doi.org/10.1016/j.jdiacomp.2006.03.004
Genest DS, Falcao S, Gutkowska J, Lavoie JL (2012) Impact of exercise training on preeclampsia: potential preventive mechanisms. Hypertension 60:1104–1109. https://doi.org/10.1161/HYPERTENSIONAHA.112.194050
Carter S, Hartman Y, Holder S, Thijssen DH, Hopkins ND (2017) Sedentary behavior and cardiovascular disease risk: mediating mechanisms. Exerc Sport Sci Rev 45:80–86. https://doi.org/10.1249/JES.0000000000000106
Fazzi C, Saunders DH, Linton K, Norman JE, Reynolds RM (2017) Sedentary behaviours during pregnancy: a systematic review. Int J Behav Nutr Phys Act 14:32. https://doi.org/10.1186/s12966-017-0485-z
Spracklen CN, Ryckman KK, Triche EW, Saftlas AF (2016) Physical activity during pregnancy and subsequent risk of preeclampsia and gestational hypertension: a case control study. Matern Child Health J 20:1193–1202. https://doi.org/10.1007/s10995-016-1919-y
Vestgaard M, Asbjornsdottir B, Ringholm L (2019) White coat hypertension in early pregnancy in women with pre-existing diabetes: prevalence and pregnancy outcomes. Diabetologia. https://doi.org/10.1007/s00125-019-05002-9
Chasan-Taber L, Schmidt MD, Roberts DE, Hosmer D, Markenson G, Freedson PS (2004) Development and validation of a pregnancy physical activity questionnaire. Med Sci Sport Exerc 36:1750–1760
Vestgaard M, Carstens Soholm J, Kjaerhus Norgaard S et al (2019) Home blood pressure in pregnancy-the upper reference limit. Blood Press Monit 24:191–198. https://doi.org/10.1097/MBP.0000000000000386
Simmons D, Devlieger R, van Assche A et al (2017) Effect of physical activity and/or healthy eating on GDM Risk: the DALI lifestyle study. J Clin Endocrinol Metab 102:903–913. https://doi.org/10.1210/jc.2016-3455
Ainsworth BE, Haskell WL, Herrmann SD et al (2011) Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 43:1575–1581. https://doi.org/10.1249/MSS.0b013e31821ece12
Norgaard SK, Vestgaard MJ, Jorgensen IL et al (2018) Diastolic blood pressure is a potentially modifiable risk factor for preeclampsia in women with pre-existing diabetes. Diabetes Res Clin Pr 138:229–237. https://doi.org/10.1016/j.diabres.2018.02.014
American College of O, Gynecologists, Task Force on Hypertension in P (2013) Hypertension in pregnancy. Report of the American College of obstetricians and gynecologists’ task force on hypertension in pregnancy. Obs Gynecol 122:1122–1131. https://doi.org/10.1097/01.AOG.0000437382.03963.88
Marsal K, Persson PH, Larsen T, Lilja H, Selbing A, Sultan B (1996) Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr 85:843–848
UNESCO (1997) United Nations educational SACO. International Standard Classification of Education: ISCED
Davenport MH, Meah VL, Ruchat S-M et al (2018) Impact of prenatal exercise on neonatal and childhood outcomes: a systematic review and meta-analysis. Br J Sports Med 52:1386–1396. https://doi.org/10.1136/bjsports-2018-099836
Guillemette L, Hay JL, Kehler DS et al (2018) Exercise in pregnancy and children’s cardiometabolic risk factors: a systematic review and meta-analysis. Sport Med open 4:35. https://doi.org/10.1186/s40798-018-0148-x
van Poppel MNM, Simmons D, Devlieger R et al (2019) A reduction in sedentary behaviour in obese women during pregnancy reduces neonatal adiposity: the DALI randomised controlled trial. Diabetologia 62:915–925. https://doi.org/10.1007/s00125-019-4842-0
Borodulin KM, Evenson KR, Wen F, Herring AH, Benson AM (2008) Physical activity patterns during pregnancy. Med Sci Sports Exerc 40:1901–1908. https://doi.org/10.1249/MSS.0b013e31817f1957
Currie S, Sinclair M, Liddle DS, Nevill A, Murphy MH (2015) Application of objective physical activity measurement in an antenatal physical activity consultation intervention: a randomised controlled trial. BMC Public Health 15:1259. https://doi.org/10.1186/s12889-015-2548-x
Acknowledgements
The authors thank the staff at Center for Pregnant Women with Diabetes, Rigshospitalet, and Center for Diabetes and Pregnancy, Odense University Hospital, for help with recruitment and data collection. We kindly thank research-midwife Maria Anna Mikkelsen for help with collection and handling of data.
Funding
NCD, BÁ and ERM were funded by Novo Nordisk Foundation. MV was funded by Rigshospitalets Research Foundation. The project was also funded by the Research Foundation between OUH and Rigshospitalet and the Exchange Foundation between OUH and Rigshospitalet. The funding sources had no influence on the study design, handling of data or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
ERM, NCD and MV contributed to the idea. NCD, MV and BA collected the data. NCD analyzed the data and wrote the first draft of the manuscript. All authors were involved in the interpretation of data, contributed to the discussion, reviewed and edited the manuscript and approved the final version. ERM is the guarantor of this work and, as such, has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest in connection with this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee—The National Committee on Health Research Ethics (H-15019186) and The Danish Data Protection Agency (2012-58-0004, RH-2015-289, I-Suite: 04305) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Pregnancy and diabetes managed by Antonio Secchi.
Rights and permissions
About this article
Cite this article
Do, N.C., Vestgaard, M., Ásbjörnsdóttir, B. et al. Physical activity, sedentary behavior and development of preeclampsia in women with preexisting diabetes. Acta Diabetol 57, 559–567 (2020). https://doi.org/10.1007/s00592-019-01459-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01459-7