Abstract
Aims
Type 2 diabetes (T2D) accelerates the decline in glomerular function; however, some individuals do not develop chronic kidney disease despite advanced age and long-lasting T2D. We aimed to phenotype patients with T2D aged 80 years or older who presented with a fully preserved kidney function.
Methods
From an Italian population of 281,217 T2D outpatients, we collected data on demographics, anthropometrics, diabetes duration, HbA1c, fasting plasma glucose, lipids, liver enzymes, estimated glomerular filtration rate (eGFR), albumin excretion rate (AER), chronic complications, and medication use. We primarily compared patients with a fully preserved kidney function (eGFR > 90 ml/min/1.73 m2 and AER < 30 mg/24 h, or G1A1) with those with mild kidney impairment (eGFR 60–90 ml/min/1.73 m2 and AER < 30 mg/24 h, or G2A1).
Results
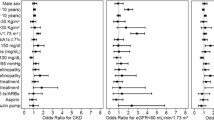
N = 113,860 had available data for eGFR and AER, 21,648 of whom were aged ≥ 80. G1A1 (n = 278) and G2A1 (n = 6647) patients represented 1.3 and 30.7% of aged T2D patients, respectively, with an average diabetes duration of 16 years. Differences between the G1A1 and G2A1 groups were entered in a multiple logistic regression analysis with and without imputation of missing data. After adjustment and in both imputed and non-imputed datasets, younger age, lower BMI and lower triglycerides were associated with fully preserved versus mildly impaired kidney function. The comparison between G1A1 and G1A2/3 yielded different results.
Conclusions
In a rare population of patients with a fully preserved kidney function despite old age and long-lasting diabetes, lower BMI and triglycerides suggest that protection from lipotoxicity may preserve kidney function over time.

Similar content being viewed by others
References
Mazzola P, Rimoldi SM, Rossi P et al (2016) Aging in Italy: the need for new welfare strategies in an old country. Gerontologist 56:383–390
England K, Azzopardi-Muscat N (2017) Demographic trends and public health in Europe. Eur J Public Health 27:9–13
Lopreite M, Mauro M (2017) The effects of population ageing on health care expenditure: a Bayesian VAR analysis using data from Italy. Health Policy 121:663–674
Vanholder R, Annemans L, Brown E et al (2017) Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat Rev Nephrol 13:393–409
Stevens LA, Li S, Wang C et al (2010) Prevalence of CKD and comorbid illness in elderly patients in the United States: results from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 55:S23–S33
Tsai CW, Ting IW, Yeh HC, Kuo CC (2017) Longitudinal change in estimated GFR among CKD patients: a 10-year follow-up study of an integrated kidney disease care program in Taiwan. PLoS One 12:e0173843
Fox CS, Matsushita K, Woodward M et al (2012) Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 380:1662–1673
Bruck K, Stel VS, Gambaro G et al (2016) CKD prevalence varies across the European general population. J Am Soc Nephrol 27:2135–2147
Pugliese G, Solini A, Bonora E et al (2014) Chronic kidney disease in type 2 diabetes: lessons from the renal insufficiency and cardiovascular events (RIACE) Italian Multicentre Study. Nutr Metab Cardiovasc Dis 24:815–822
Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 14:88–98
Canaud B, Tong L, Tentori F et al (2011) Clinical practices and outcomes in elderly hemodialysis patients: results from the dialysis outcomes and practice patterns study (DOPPS). Clin J Am Soc Nephrol 6:1651–1662
Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE (2009) Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 361:1539–1547
Thomas B, Matsushita K, Abate KH et al (2017) Global cardiovascular and renal outcomes of reduced GFR. J Am Soc Nephrol 28:2167–2179
Fung CS, Wan EY, Chan AK, Lam CL (2017) Association of estimated glomerular filtration rate and urine albumin-to-creatinine ratio with incidence of cardiovascular diseases and mortality in Chinese patients with type 2 diabetes mellitus—a population-based retrospective cohort study. BMC Nephrol 18:47
Fadini GP, Zatti G, Baldi I et al (2018) Use and effectiveness of dapagliflozin in routine clinical practice: an Italian multicentre retrospective study. Diabetes Obes Metab 20:1781–1786. https://doi.org/10.1111/dom.13280
Fadini GP, Zatti G, Consoli A, Bonora E, Sesti G, Avogaro A (2017) Rationale and design of the DARWIN-T2D (DApagliflozin Real World evIdeNce in Type 2 Diabetes): a multicenter retrospective nationwide Italian study and crowdsourcing opportunity. Nutr Metab Cardiovasc Dis 27:1089–1097
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
National Kidney Foundation (2018) https://www.kidneyorg/professionals/explore-your-knowledge/how-to-classify-ckd. Accessed April 2018
Rubin R (1996) Multiple imputation after 18+ years. J Am Stat Assoc 91:473–489
Penno G, Solini A, Zoppini G et al (2015) Hypertriglyceridemia Is independently associated with renal, but not retinal complications in subjects with type 2 diabetes: a cross-sectional analysis of the renal insufficiency and cardiovascular events (RIACE) Italian Multicenter Study. PLoS One 10:e0125512
Russo GT, De Cosmo S, Viazzi F et al (2016) Plasma triglycerides and HDL-C levels predict the development of diabetic kidney disease in subjects with type 2 diabetes: the AMD annals initiative. Diabetes Care 39:2278–2287
Tsuruya K, Yoshida H, Nagata M et al (2015) Impact of the triglycerides to high-density lipoprotein cholesterol ratio on the incidence and progression of CKD: a longitudinal study in a large Japanese population. Am J Kidney Dis 66:972–983
Lanktree MB, Theriault S, Walsh M, Pare G (2018) HDL cholesterol, LDL cholesterol, and triglycerides as risk factors for CKD: a Mendelian randomization study. Am J Kidney Dis 71:166–172
Scott D, Cumming R, Naganathan V et al (2018) Associations of sarcopenic obesity with the metabolic syndrome and insulin resistance over five years in older men: the concord health and ageing in men project. Exp Gerontol 108:99–105
Ferrara LA, Capaldo B, Mancusi C et al (2014) Cardiometabolic risk in overweight subjects with or without relative fat-free mass deficiency: the strong heart study. Nutr Metab Cardiovasc Dis 24:271–276
Izquierdo-Lahuerta A, Martinez-Garcia C, Medina-Gomez G (2016) Lipotoxicity as a trigger factor of renal disease. J Nephrol 29:603–610
Karalliedde J, Gnudi L (2016) Diabetes mellitus, a complex and heterogeneous disease, and the role of insulin resistance as a determinant of diabetic kidney disease. Nephrol Dial Transpl 31:206–213
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351:1296–1305
Targher G, Byrne CD (2017) Non-alcoholic fatty liver disease: an emerging driving force in chronic kidney disease. Nat Rev Nephrol 13:297–310
Hwang ST, Cho YK, Yun JW et al (2010) Impact of non-alcoholic fatty liver disease on microalbuminuria in patients with prediabetes and diabetes. Intern Med J 40:437–442
Avogaro A, Fadini GP (2014) The effects of dipeptidyl peptidase-4 inhibition on microvascular diabetes complications. Diabetes Care 37:2884–2894
Tella SH, Rendell MS (2015) DPP-4 inhibitors: focus on safety. Expert Opin Drug Saf 14:127–140
Russo GT, De Cosmo S, Viazzi F et al (2018) Diabetic kidney disease in the elderly: prevalence and clinical correlates. BMC Geriatr 18:38
Solini A, Penno G, Bonora E et al (2013) Age, renal dysfunction, cardiovascular disease, and antihyperglycemic treatment in type 2 diabetes mellitus: findings from the Renal Insufficiency and Cardiovascular Events Italian Multicenter Study. J Am Geriatr Soc 61:1253–1261
Vinik A (2011) The question is, my dear watson, why did the dog not bark? The Joslin 50-year medalist study. Diabetes Care 34:1060–1063
Qi W, Li Q, Gordin D, King GL (2018) Preservation of renal function in chronic diabetes by enhancing glomerular glucose metabolism. J Mol Med (Berl) 96:373–381
Hirst JA, Montes MDV, Taylor CJ et al (2018) Impact of a single eGFR and eGFR-estimating equation on chronic kidney disease reclassification: a cohort study in primary care. Br J Gen Pract 68:e524–e530. https://doi.org/10.3399/bjgp18X697937
Pugliese G, Solini A, Fondelli C et al (2011) Reproducibility of albuminuria in type 2 diabetic subjects. Findings from the renal insufficiency and cardiovascular events (RIACE) study. Nephrol Dial Transpl 26:3950–3954
Penno G, Solini A, Bonora E et al (2018) Defining the contribution of chronic kidney disease to all-cause mortality in patients with type 2 diabetes: the renal insufficiency and cardiovascular events (RIACE) Italian Multicenter Study. Acta Diabetol 55:603–612
Acknowledgements
We wish to thank Alessia Russo, Italian Diabetes Society, for the invaluable technical support.
Agostino Consoli and Gloria Formoso (Dipartimento di Medicina e Scienze dell’Invecchiamento—Università Degli studi G. D’Annunzio di Chieti-Pescara); Giovanni Grossi (Ospedale San Francesco di Paola—Azienda Sanitaria Provinciale di Cosenza); Achiropita Pucci (Azienda Sanitaria Provinciale di Cosenza); Giorgio Sesti and Francesco Andreozzi (Azienda Ospedaliero Universitaria di Catanzaro); Giuseppe Capobianco (Azienda Sanitaria Locale Napoli 2 Nord); Adriano Gatti (Ospedale San Gennaro dei Poveri—Azienda Sanitaria Locale Napoli 1 Centro); Riccardo Bonadonna, Ivana Zavaroni and Alessandra Dei Cas (Azienda Ospedaliero Universitaria di Parma); Giuseppe Felace (Ospedale di Spilimbergo—Azienda per l’Assistenza Sanitaria n.5 Friuli Occidentale); Patrizia Li Volsi (Ospedale di Pordenone—Azienda per l’Assistenza Sanitaria n.5 Friuli Occidentale); Raffaella Buzzetti and Gaetano Leto (Ospedale Santa Maria Goretti—Azienda Sanitaria Locale di Latina); Gian Pio Sorice (Fondazione Policlinico Universitario A. Gemelli, Roma); Paola D’Angelo (Ospedale Sandro Pertini—Azienda Sanitaria Locale Roma 2); Susanna Morano (Azienda Ospedaliera Universitaria Policlinico Umberto I, Roma); Antonio Carlo Bossi (Ospedale di Treviglio—Azienda Socio Sanitaria Territoriale Bergamo Ovest); Edoardo Duratorre (Ospedale Luini Confalonieri di Luino—Azienda Socio Sanitaria Territoriale Sette Laghi); Ivano Franzetti (Ospedale Sant’Antonio Abate di Gallarate—Azienda Socio Sanitaria Territoriale Valle Olona); Paola Silvia Morpurgo (Ospedale Fatebenefratelli—Azienda Socio Sanitaria Territoriale Fatebenefratelli Sacco); Emanuela Orsi (Fondazione IRCCS Ca’ Granda—Ospedale Maggiore Policlinico di Milano); Fabrizio Querci (Ospedale Pesenti Fenaroli di Alzano Lombardo—Azienda Socio Sanitaria Territoriale Bergamo Est); Massimo Boemi† and Federica D’Angelo (Presidio Ospedaliero di Ricerca INRCA-IRCCS di Ancona); Massimiliano Petrelli (Azienda Ospedaliero Universitaria Ospedali Riuniti di Ancona); Gianluca Aimaretti and Ioannis Karamouzis (Azienda Ospedaliero Universitaria Maggiore della Carità di Novara); Franco Cavalot (Azienda Ospedaliero Universitaria San Luigi Gonzaga, Orbassano); Giuseppe Saglietti† (Ospedale Madonna del Popolo di Omegna—Azienda Sanitaria Locale Verbano Cusio Ossola); Giuliana Cazzetta (Casa della Salute, Ugento—Distretto Socio Sanitario Gagliano del Capo—Azienda Sanitaria Locale di Lecce); Silvestre Cervone (Presidio ospedaliero San Marco in Lamis—Distretto Socio Sanitario San Marco in Lamis—Azienda Sanitaria Locale di Foggia); Eleonora Devangelio (Distretto Socio Sanitario di Massafra—Azienda Sanitaria Locale di Taranto); Olga Lamacchia (Azienda Ospedaliero Universitaria Ospedali Riuniti di Foggia); Salvatore Arena (Ospedale Umberto I—Azienda Sanitaria Provinciale di Siracusa); Antonino Di Benedetto (Azienda Ospedaliera Universitaria Policlinico G. Martino di Messina); Lucia Frittitta (Azienda Ospedaliera di Rilievo Nazionale e di Alta Specializzazione Garibaldi di Catania); Carla Giordano (Azienda Universitaria Policlinico Paolo Giaccone di Palermo); Salvatore Piro (Azienda Ospedaliera di Rilievo Nazionale e di Alta Specializzazione Garibaldi di Catania); Manfredi Rizzo, Roberta Chianetta and Carlo Mannina (Azienda Universitaria Policlinico Paolo Giaccone di Palermo); Roberto Anichini (Ospedale San Jacopo di Pistoia—Azienda USL Toscana Centro); Giuseppe Penno (Azienda Ospedaliero Universitaria Pisana); Anna Solini (Azienda Ospedaliera Universitaria Pisana); Bruno Fattor (Comprensorio Sanitario di Bolzano—Azienda Sanitaria della Provincia Autonoma di Bolzano); Enzo Bonora and Massimo Cigolini (Azienda Ospedaliero Universitaria Integrata di Verona); Annunziata Lapolla and Nino Cristiano Chilelli (Complesso Socio Sanitario Ai Colli—Azienda ULSS n.6 Euganea); Maurizio Poli (Ospedale Girolamo Fracastoro di San Bonifacio—Azienda ULSS n.9 Scaligera); Natalino Simioni and Vera Frison (Ospedale di Cittadella—Azienda ULSS n.6 Euganea); Carmela Vinci (Azienda ULSS n.4 Veneto Orientale).
Funding
The study was supported by the Italian Diabetes Society.
Author information
Authors and Affiliations
Consortia
Contributions
Study design: GPF and AS. Data collection and analysis: GPF, AS, AA, GZ, MLM, IK, LF, ADB. Manuscript writing GPF, AS, AA. Manuscript revision GZ, MLM, LF, ADB, IK. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
GPF received Grant support, lecture or advisory board fees from AstraZeneca, Boehringer-Ingelheim, Eli Lilly, NovoNordisk, Sanofi, Genzyme, Abbott, Novartis, Merck Sharp and Dohme. AS received research Grants from Astra Zeneca and served as advisory board member for Boehringer-Ingelheim and Eli-Lilly. ADB received research grants from NovoNordisk and AstraZeneca, and lecture fees from Boehringer-Ingelheim, Eli-Lilly, Sanofi, Lifescan, Menarini diagnostics. LF received research grant from Therascience, lecture or advisory board fees from Eli-Lilly, Novo-Nordisk, Takeda, AstraZeneca. AA received research grants, lecture or advisory board fees from Merck Sharp and Dome, AstraZeneca, Novartis, Boeringher-Ingelheim, Sanofi, Mediolanum, Janssen, NovoNordisk. GZ, MLM and IK declare no conflict of interest.
Ethical standard
The study was approved by ethical committees of participanting Centers and it was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki.
Informed consent
In agreement with National regulations on data protection and privacy, no informed consent was collected because the database was anonymous.
Additional information
Managed by Massimo Porta.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fadini, G.P., Solini, A., Manca, M.L. et al. Phenotyping normal kidney function in elderly patients with type 2 diabetes: a cross-sectional multicentre study. Acta Diabetol 55, 1121–1129 (2018). https://doi.org/10.1007/s00592-018-1194-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1194-z