Abstract
Background
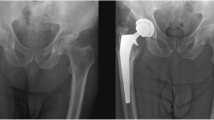
Heterotopic ossification (HO) formation has been increasingly recognized as a complication of major orthopedic surgeries, particularly total hip arthroplasty (THA). Though, the overall incidence of HO following THA has been well-documented, it is often not reported by severity or by surgical approach.
Questions/purposes.
(1) What are the demographics of patients with HO? (2) What is the severity of HO following THA using the Brooker classification? (3) What is the incidence and class of HO following different THA approaches (anterior, posterior, posterolateral, anterolateral, superior, lateral, trans-gluteal)? (4) What are the number and training level of surgeons who performed each procedure?
Methods
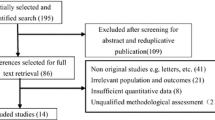
The PubMed, Embase, and Web of Science databases were queried, and PRISMA guidelines were followed. Qualitative and quantitative analyses were performed using Microsoft Excel.
Results
We isolated 26 studies evaluating 6512 total hip arthroplasties (THA). The mean HO percentage overall was 28.8%, mostly Class I (54.2%) or Class II (29.6%). The highest percentage of HO was associated with the modified direct lateral (57.2%) and the traditional lateral (34.6%) approaches. The lowest HO percentages were identified following posterolateral (12.8%) and direct superior approaches (1%). Most studies reported a singular senior surgeon operating within the same approach for all patients.
Conclusions
The traditional lateral and modified direct lateral approaches to THA resulted in the highest percentage of HO postoperatively. However, most ossification cases were not clinically significant and did not strongly affect overall patient morbidity. Further studies are warranted to identify an association between severity of ossification and different arthroplasty approaches.


Similar content being viewed by others
References
Ranganathan K et al (2015) Heterotopic ossification: basic-science principles and clinical correlates. J Bone Jt Surg Am 97:1101–1111. https://doi.org/10.2106/jbjs.N.01056
Popovic M et al (2014) Radiotherapy for the prophylaxis of heterotopic ossification: a systematic review and meta-analysis of published data. Radiother Oncol 113:10–17. https://doi.org/10.1016/j.radonc.2014.08.025
Meyers C, Lisiecki J, Miller S et al (2019) Heterotopic ossification: a comprehensive review. JBMR Plus 3(4):10172. https://doi.org/10.1002/jbm4.101723
Chémaly O, Hebert-Davies J, Rouleau DM, Benoit B, Laflamme GY (2013) Heterotopic ossification following total hip replacement for acetabular fractures. Bone Jt J 95:95–100. https://doi.org/10.1302/0301-620x.95b1.29721
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Jt Surg Am 55(1629):1632
Di Benedetto P et al (2019) Heterotopic ossification in primary total hip arthroplasty: which is the role of drainage? Acta Biomed 90:92–97. https://doi.org/10.23750/abm.v90i1-S.8077
Kocic M, Lazovic M, Mitkovic M, Djokic B (2010) Clinical significance of the heterotopic ossification after total hip arthroplasty. Orthopedics 33:16. https://doi.org/10.3928/01477447-20091124-13
Łęgosz P et al (2019) Heterotopic ossification: a challenging complication of total hip arthroplasty: risk factors, diagnosis, prophylaxis, and treatment. Biomed Res Int 2019:3860142. https://doi.org/10.1155/2019/3860142
Aggarwal VK et al (2019) Surgical approach significantly affects the complication rates associated with total hip arthroplasty. Bone Jt J 101(646):651. https://doi.org/10.1302/0301-620x.101b6.Bjj-2018-1474.R1
Aggarwal VK, Iorio R, Zuckerman JD, Long WJ (2020) Surgical approaches for primary total hip arthroplasty from charnley to now: the quest for the best approach. JBJS Rev 8:58. https://doi.org/10.2106/JBJS.RVW.19.00058
Slim K et al (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Follow Up, Hip and Knee Care. AAHKS Hip and Knee Care. 2023 https://hipknee.aahks.org/dont-take-your-new-joint-for-granted-follow-up-care/
Ateschrang A et al (2014) Long-term results using the straight tapered femoral cementless hip stem in total hip arthroplasty: a minimum of twenty-year follow-up. J Arthroplast 29:1559–1565. https://doi.org/10.1016/j.arth.2014.02.015
Busch A et al (2020) Total hip arthroplasty following acetabular fracture: a clinical and radiographic outcome analysis of 67 patients. Arch Orthop Trauma Surg 140:331–341. https://doi.org/10.1007/s00402-019-03272-x
Choy WS, Cha YH, Jeon CY, Lee KS, Kim HY (2018) A minimum ten years of follow-up of alumina head on delta liner total hip arthroplasty. J Arthroplast 33:470–476. https://doi.org/10.1016/j.arth.2017.08.043
Edwards DS, Barbur SA, Bull AM, Stranks GJ (2015) Posterior mini-incision total hip arthroplasty controls the extent of post-operative formation of heterotopic ossification. Eur J Orthop Surg Traumatol 25:1051–1055. https://doi.org/10.1007/s00590-015-1646-x
Fischer C et al (2021) Retrospective clinical and radiological outcomes of total hip arthroplasty in 51 patients after a mean 8.2 years using the nanos® short-stem prosthesis. Surg Technol Int 39:348–353. https://doi.org/10.52198/21.STI.39.OS1473
Gofton W et al (2019) Ten-year experience with the anterior approach to total hip arthroplasty at a tertiary care center. J Arthroplast 35:1281–1289. https://doi.org/10.1016/j.arth.2019.12.025
Hartford JM, Bellino MJ (2017) The learning curve for the direct anterior approach for total hip arthroplasty: a single surgeon’s first 500 cases. Hip Int 27:483–488. https://doi.org/10.5301/hipint.5000488
Hayashi D et al (2019) Severity of heterotopic ossification in patients following surgery for hip fracture: a retrospective observational study. BMC Musculoskelet Disord 20:348. https://doi.org/10.1186/s12891-019-2725-7
Hürlimann M et al (2017) Influence of surgical approach on heterotopic ossification after total hip arthroplasty - is minimal invasive better? a case control study. BMC Musculoskelet Disord 18:27. https://doi.org/10.1186/s12891-017-1391-x
Kutzner KP et al (2017) Incidence of heterotopic ossification in minimally invasive short-stem THA using the modified anterolateral approach. Hip Int 27:162–168. https://doi.org/10.5301/hipint.5000448
Lavernia CJ, Contreras JS, Villa JM, Rossi MD (2014) Celecoxib and heterotopic bone formation after total hip arthroplasty. J Arthroplast 29:390–392. https://doi.org/10.1016/j.arth.2013.06.039
Leunig M et al (2018) Skin crease “bikini” incision for the direct anterior approach in total hip arthroplasty: a two- to four-year comparative study in 964 patients. Bone Jt J 100(853):861. https://doi.org/10.1302/0301-620X.100B7.BJJ-2017-1200.R2
Malhotra R, Gautam D (2019) Acute total hip arthroplasty in acetabular fractures using modern porous metal cup. J Orthop Surg (Hong Kong) 27:2309499019855438. https://doi.org/10.1177/2309499019855438
Malhotra R, Kumar V (2016) Mid-term outcome of total hip arthroplasty using a short stem. J Orthop Surg (Hong Kong) 24:323–327. https://doi.org/10.1177/1602400310
Marchica D, Gallazzi E, Materazzi G, Battaglia GA, Zagra L (2018) MRI findings, metal ion levels and clinical outcome of a complete series of large metal on metal THA: what’s really going on? Hip Int 28:48–53. https://doi.org/10.1177/1120700018813223
Mitchell RJ, Kay AB, Smith KM, Murphy SB, Le DT (2019) Early results of displaced femoral neck fragility fractures treated with supercapsular percutaneous-assisted total hip arthroplasty. Arthroplast Today 5:193–196. https://doi.org/10.1016/j.artd.2019.02.003
Newman EA, Holst DC, Bracey DN, Russell GB, Lang JE (2016) Incidence of heterotopic ossification in direct anterior vs posterior approach to total hip arthroplasty: a retrospective radiographic review. Int Orthop 40:1967–1973. https://doi.org/10.1007/s00264-015-3048-4
Patil S, Luis C, Finn H (2017) Porous femoral fixation in total hip arthroplasty with short anatomical stem: radiographic evaluation. Clin Orthop Surg 9:255–262. https://doi.org/10.4055/cios.2017.9.3.255
Rashed RA et al (2020) Is dual mobility cup total hip replacement associated with increased incidence of heterotopic ossification compared to conventional total hip replacements in fracture neck of femur patients? Injury 51:2676–2681. https://doi.org/10.1016/j.injury.2020.07.045
Rüdiger HA et al (2020) The impact of heterotopic ossification on self-reported outcomes after total hip arthroplasty using the direct anterior approach. J Bone Jt Surg Am 102:91–98. https://doi.org/10.2106/jbjs.20.00071
Syed MA, Hutt NJ, Shah N, Edge AJ (2015) Hydroxyapatite ceramic-coated femoral components in young patients followed up for 17 to 25 years: an update of a previous report. Bone Jt J 97(749):754. https://doi.org/10.1302/0301-620x.97b6.35278
Tippets DM et al (2014) Incidence of heterotopic ossification in direct anterior total hip arthroplasty: a retrospective radiographic review. J Arthroplast 29:1835–1838. https://doi.org/10.1016/j.arth.2014.04.027
Tsiridis E, Kenanidis E, Potoupnis M, Sayegh FE (2020) Direct superior approach with standard instrumentation for total hip arthroplasty: safety and efficacy in a prospective 200-case series. Hip Int 30:552–558. https://doi.org/10.1177/1120700019843120
White PB et al (2018) Incidence of heterotopic ossification following a multimodal pain protocol in total hip arthroplasty with the posterior approach. Orthopedics 41:92–97. https://doi.org/10.3928/01477447-20171102-01
Zhen P et al (2017) Developmental hip dysplasia treated by total hip arthroplasty using a cementless wagner cone stem in young adult patients with a small physique. BMC Musculoskelet Disord 18:192. https://doi.org/10.1186/s12891-017-1554-9
Fang M et al (2015) The effect of advancing age on total joint replacement outcomes. Geriatr Orthop Surg Rehabil 6:173–179. https://doi.org/10.1177/2151458515583515
Hagman DS et al (2022) Primary THA using thin polyethylene liners and large femoral heads: a minimum 5-year follow-up. J Arthroplast 37:S588–S591. https://doi.org/10.1016/j.arth.2022.02.117
Pollock M et al (2016) Outpatient total hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty: a systematic review of the literature. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.16.00002
Zhu Y et al (2015) Incidence and risk factors for heterotopic ossification after total hip arthroplasty: a meta-analysis. Arch Orthop Trauma Surg 135:1307–1314. https://doi.org/10.1007/s00402-015-2277-8
Jauregui JJ et al (2020) Acute total hip arthroplasty for older patients with acetabular fractures: a meta-analysis. J Clin Orthop Trauma 11:976–982. https://doi.org/10.1016/j.jcot.2020.01.003
Fessy MH et al (2017) What are the risk factors for dislocation in primary total hip arthroplasty? a multicenter case-control study of 128 unstable and 438 stable hips. Orthop Traumatol Surg Res 103:663–668. https://doi.org/10.1016/j.otsr.2017.05.014
Shimono K et al (2011) Potent inhibition of heterotopic ossification by nuclear retinoic acid receptor-γ agonists. Nat Med 17:454–460. https://doi.org/10.1038/nm.2334
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors did not receive support from any organization for the submitted work. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Herzberg, R., Tracey, O.C., Tahvilian, S. et al. Incidence of heterotopic ossification following total hip arthroplasty by approach: a systematic review. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-03896-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-03896-9