Abstract
Purpose
There is a common belief among some shoulder surgeons that the increased utilization of reverse shoulder arthroplasty (RSA) is driven by the operation being performed in younger patients. The primary purpose of this study was to evaluate the change in patient age at the time of primary RSA in the USA.
Methods
All patients undergoing primary RSA (January 2011–June 2018) were identified in the Mariner database. The mean age at the time of primary RSA was evaluated for each patient and assessed in 6-month intervals. A longitudinal comparison over time was performed for all patients.
Results
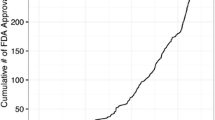
A total of 56,141 primary RSA were evaluated, with the mean age increasing from 69 in the 2011 to 71 in 2018 (p < 0.001). The largest increase in RSA utilization occurred in patients > 70 (1092 in 2011 to 3499 in 2018), with patients < 50 years demonstrating the slowest growth (13 in 2011 to 65 in 2018). However, when evaluated by percentage increase from 2011 to 2018, RSA volumes for patients < 60 have increased 390% compared to 220% for those > 70 years (p < 0.001).
Conclusion
RSA continues to be performed at a similar mean age despite expanded indications and surgeon comfort. However, patients < 60 years have had a greater increase in utilization compared to patients > 70 years. The volumetric growth of RSA has largely been driven by the older population, but younger patients have shown a higher percentage of growth, which may explain the generalized observation that RSA is performed in younger patients.
Level of Evidence
Level III; Retrospective comparative study; Treatment study.





Similar content being viewed by others
References
Chalmers PN, Salazar DH, Romeo AA et al (2018) Comparative utilization of reverse and anatomic total shoulder arthroplasty: a comprehensive analysis of a high-volume center. J Am Acad Orthop Surg 26:e504–e510. https://doi.org/10.5435/JAAOS-D-17-00075
Schairer WW, Nwachukwu BU, Lyman S et al (2015) National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 24:91–97. https://doi.org/10.1016/j.jse.2014.08.026
Wagner ER, Farley KX, Higgins I et al (2020) The incidence of shoulder arthroplasty: rise and future projections compared with hip and knee arthroplasty. J Shoulder Elbow Surg 29:2601–2609. https://doi.org/10.1016/j.jse.2020.03.049
Best MJ, Aziz KT, Wilckens JH et al (2021) Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 30:1159–1166. https://doi.org/10.1016/j.jse.2020.08.010
Harjula JNE, Paloneva J, Haapakoski J et al (2018) Increasing incidence of primary shoulder arthroplasty in Finland – a nationwide registry study. BMC Musculoskelet Disord 19:245. https://doi.org/10.1186/s12891-018-2150-3
Bufquin T, Hersan A, Hubert L, Massin P (2007) Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 89:516–520. https://doi.org/10.1302/0301-620X.89B4.18435
Mizuno N, Denard PJ, Raiss P, Walch G (2013) Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am 95:1297–1304. https://doi.org/10.2106/JBJS.L.00820
Schoch B, Werthel J-D, Sperling JW et al (2016) Is shoulder arthroplasty an option for charcot arthropathy? Int Orthop 40:2589–2595. https://doi.org/10.1007/s00264-016-3309-x
Statz JM, Schoch BS, Sanchez-Sotelo J et al (2017) Shoulder arthroplasty for locked anterior shoulder dislocation: a role for the reversed design. Int Orthop 41:1227–1234. https://doi.org/10.1007/s00264-017-3450-1
Ernstbrunner L, Suter A, Catanzaro S et al (2017) Reverse total shoulder arthroplasty for massive, irreparable rotator cuff tears before the age of 60 years: long-term results. J Bone Joint Surg Am 99:1721–1729. https://doi.org/10.2106/JBJS.17.00095
Leathers MP, Ialenti MN, Feeley BT et al (2018) Do younger patients have better results after reverse total shoulder arthroplasty? J Shoulder Elbow Surg 27:S24–S28. https://doi.org/10.1016/j.jse.2017.11.014
Monir JG, Abeyewardene D, King JJ et al (2020) Reverse shoulder arthroplasty in patients younger than 65 years, minimum 5-year follow-up. J Shoulder Elbow Surg 29:e215–e221. https://doi.org/10.1016/j.jse.2019.10.028
Otto RJ, Clark RE, Frankle MA (2017) Reverse shoulder arthroplasty in patients younger than 55 years: 2- to 12-year follow-up. J Shoulder Elbow Surg 26:792–797. https://doi.org/10.1016/j.jse.2016.09.051
Samuelsen BT, Wagner ER, Houdek MT et al (2017) Primary reverse shoulder arthroplasty in patients aged 65 years or younger. J Shoulder Elbow Surg 26:e13–e17. https://doi.org/10.1016/j.jse.2016.05.026
Sershon RA, Van Thiel GS, Lin EC et al (2014) Clinical outcomes of reverse total shoulder arthroplasty in patients aged younger than 60 years. J Shoulder Elbow Surg 23:395–400. https://doi.org/10.1016/j.jse.2013.07.047
Ammitzboell M, Baram A, Brorson S et al (2019) Poor patient-reported outcome after shoulder replacement in young patients with cuff-tear arthropathy: a matched-pair analysis from the Danish Shoulder Arthroplasty Registry. Acta Orthop 90:119–122. https://doi.org/10.1080/17453674.2018.1563855
Schoch BS, Vigan M, Roche C et al (2020) Deltoid fatigue: a longitudinal assessment of reverse shoulder arthroplasty over time. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2020.08.038
Bacle G, Nové-Josserand L, Garaud P, Walch G (2017) Long-term outcomes of reverse total shoulder arthroplasty: a follow-up of a previous study. J Bone Joint Surg Am 99:454–461. https://doi.org/10.2106/JBJS.16.00223
Guery J, Favard L, Sirveaux F et al (2006) Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am 88:1742–1747. https://doi.org/10.2106/JBJS.E.00851
Schoch BS, Vigan M, Roche C et al (2021) Deltoid fatigue part 2: a longitudinal assessment of anatomic total shoulder arthroplasty over time. J Shoulder Elbow Surg S1058–2746(21):00635–00642. https://doi.org/10.1016/j.jse.2021.07.019
Farley KX, Wilson JM, Kumar A et al (2021) Prevalence of shoulder arthroplasty in the United States and the increasing burden of revision shoulder arthroplasty. JB JS Open Access 6(e20):00156. https://doi.org/10.2106/JBJS.OA.20.00156
Wright MA, Keener JD, Chamberlain AM (2019) Comparison of clinical outcomes after anatomic total shoulder arthroplasty and reverse shoulder arthroplasty in patients 70 years and older with glenohumeral osteoarthritis and an intact rotator cuff. J Am Acad Orthop Surg. https://doi.org/10.5435/JAAOS-D-19-00166
Kang JR, Dubiel MJ, Cofield RH et al (2019) Primary reverse shoulder arthroplasty using contemporary implants is associated with very low reoperation rates. J Shoulder Elbow Surg 28:S175–S180. https://doi.org/10.1016/j.jse.2019.01.026
Profile of Older Americans (2017). https://acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2017OlderAmericansProfile.pdf. Accessed 3 May 2022
Reams RC, Vigan M, Wright TW et al (2020) A 10-year experience with reverse shoulder arthroplasty: are we operating earlier? J Shoulder Elbow Surg 29:S126–S133. https://doi.org/10.1016/j.jse.2020.04.040
McLean AS, Price N, Graves S et al (2019) Nationwide trends in management of proximal humeral fractures: an analysis of 77,966 cases from 2008 to 2017. J Shoulder Elbow Surg 28:2072–2078. https://doi.org/10.1016/j.jse.2019.03.034
Sayegh MJ, Nixon RA, Perfetti DC et al (2020) Changing trends in the management of proximal humerus fractures in New York State. J Orthop 21:127–130. https://doi.org/10.1016/j.jor.2020.03.001
Collin P, Hervé A, Walch G et al (2019) Mid-term results of reverse shoulder arthroplasty for glenohumeral osteoarthritis with posterior glenoid deficiency and humeral subluxation. J Shoulder Elbow Surg 28:2023–2030. https://doi.org/10.1016/j.jse.2019.03.002
Harmsen S, Casagrande D, Norris T (2017) “Shaped” humeral head autograft reverse shoulder arthroplasty : treatment for primary glenohumeral osteoarthritis with significant posterior glenoid bone loss (B2, B3, and C type). Orthopade 46:1045–1054. https://doi.org/10.1007/s00132-017-3497-0
Funding
This study received no outside funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Schoch is a paid consultant for Exactech, Inc. He receives royalties from Exactech Dr. Wright receives royalties from Exactech, Inc., and Wolters Kluwer Health—Lippincott Williams & Wilkins. He is also a paid consultant with Exactech, Inc. Dr. King owns stock in Pacira Phamaceuticals and is a paid consultant with Exactech, Inc. Dr. Werthel receives royalties from FH orthopedics. Dr. Brockmeier is a paid consultant for Exactech and Arthrex and receives royalties from Zimmer Biomet and Exactech. Dr. Werner is a paid consultant for Arthrex. He receives research support from Arthrex, Biomet, Exactech and Flexion Therapeutics.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Rights and permissions
About this article
Cite this article
Schoch, B.S., King, J.J., Wright, T.W. et al. Patient age at time of reverse shoulder arthroplasty remains stable over time: a 7.5-year trend evaluation. Eur J Orthop Surg Traumatol 33, 993–1001 (2023). https://doi.org/10.1007/s00590-022-03227-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03227-w