Abstract
Background
Candida periprosthetic joint infections (PJIs) are a rare cause of prosthesis revision with severe consequences and challenging treatment. This study aims to produce a systematic analysis of types of treatment and outcome of knee Candida PJIs and their correlation with specific pathogen species.
Methods
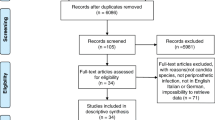
During April 2021, a literature search was performed according to PRISMA (Preferred Reporting Item for Systematic Reviews and Meta-Analyses) guideline. Reviewers used the Oxford Level of Evidence (LoE) and Methodological index for non-randomized studies (MINORS) score. Modal value of surgical, pharmacological treatment and outcome along with the correlation between types of treatment and outcome was calculated through Chi-square or Fisher exact test.
Results
In total, 115 cases were collected through 51 articles, identifying 116 pathogens. Candida albicans was the most frequent pathogen. Analysis of LoE reveals 40 LoE 5 and 11 LoE 4. Thirteen patients underwent one-stage revision, 46 patients two-stage revision, 6 patients resection arthroplasty and arthrodesis, 4 patients long-term antifungal therapy, and 3 patients debridement with prosthesis retention. Global rate of success was 85.14%. Modal distribution revealed a preference for two-stage revision and Fluconazole in medical therapy. No difference in terms of fungal eradication was found among Candida species (p = 0.503) and for treatments except for two-stage revision and resection arthroplasty (p = 0.0125) or debridement with implant retention (p = 0.0498), and the rest of procedures and resection arthroplasty (0.0192). MINORS score was poor.
Conclusions
Analysis of the literature did not highlight any difference between types of surgical treatment and pathogens in terms of relapse or infection eradication. However, two-stage replacement may be preferred, allowing healing of infection in most cases.

Similar content being viewed by others
Availability of data and materials
Data were uploaded as supplementary materials.
Change history
11 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00590-022-03239-6
References
Pulido L, Ghanem E, Joshi A et al (2008) Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res 466:1710–1715. https://doi.org/10.1007/s11999-008-0209-4
Del Pozo JL, Patel R (2009) Infection associated with prosthetic joints. N Engl J Med 361:787–794. https://doi.org/10.1056/NEJMcp0905029
Cobo F, Rodríguez-Granger J, Sampedro A et al (2017) Candida prosthetic joint infection. A review of treatment methods. J Bone Jt Infect 2:114–121. https://doi.org/10.7150/jbji.17699
Geng L, Xu M, Yu L et al (2016) Risk factors and the clinical and surgical features of fungal prosthetic joint infections: a retrospective analysis of eight cases. Exp Ther Med 12:991–999. https://doi.org/10.3892/etm.2016.3353
Osmon DR, Berbari EF, Berendt AR et al (2013) Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 56:e1–e25. https://doi.org/10.1093/cid/cis803
Klement MR, Siddiqi A, Rock JM et al (2017) Are all periprosthetic joint infections the same? Evaluating major versus minor criteria. J Arthroplasty. https://doi.org/10.1016/j.arth.2017.12.010
Parvizi J, Della Valle CJ (2010) AAOS Clinical Practice Guideline: diagnosis and treatment of periprosthetic joint infections of the hip and knee. J Am Acad Orthop Surg 18:771–772
Workgroup Convened by the Musculoskeletal Infection Society (2011) New definition for periprosthetic joint infection. J Arthroplasty 26:1136–1138. https://doi.org/10.1016/j.arth.2011.09.026
Spilf O, Collège des Universitaires de Maladies Infectieuses et Tropicales (CMIT), Groupe de Pathologie Infectieuse Pédiatrique (GPIP) et al (2010) Recommendations for bone and joint prosthetic device infections in clinical practice (prosthesis, implants, osteosynthesis). Médecine Mal Infect 40:185–211. https://doi.org/10.1016/j.medmal.2009.12.009
Minassian AM, Osmon DR, Berendt AR (2014) Clinical guidelines in the management of prosthetic joint infection. J Antimicrob Chemother 69:i29–i35. https://doi.org/10.1093/jac/dku253
Esposito S, Leone S, Bassetti M et al (2009) Italian guidelines for the diagnosis and infectious disease management of osteomyelitis and prosthetic joint infections in adults. Infection 37:478–496. https://doi.org/10.1007/s15010-009-8269-2
Kuiper JWP, van den Bekerom MPJ, van der Stappen J et al (2013) 2-stage revision recommended for treatment of fungal hip and knee prosthetic joint infections. Acta Orthop 84:517–523. https://doi.org/10.3109/17453674.2013.859422
Klatte TO, Kendoff D, Kamath AF et al (2014) Single-stage revision for fungal peri-prosthetic joint infection: a single-centre experience. Bone Joint J 96-B:492–496. https://doi.org/10.1302/0301-620X.96B4.32179
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 62:e1-34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Wouthuyzen-Bakker M, Nijman JM, Kampinga GA et al (2017) Efficacy of antibiotic suppressive therapy in patients with a prosthetic joint infection. J Bone Jt Infect 2:77–83. https://doi.org/10.7150/jbji.17353
OCEBM Levels of Evidence Working Group (2011) The Oxford 2011 levels of evidence. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
MacGregor R, Schimmer B, Steinberg M (1979) Results of combined amphotericin B-5-fluorcytosine therapy for prosthetic knee joint infected with Candida parapsilosis. J Rheumatol 6:451–455
Goodman JS, Seibert DG, Reahl GE, Geckler RW (1983) Fungal infection of prosthetic joints: a report of two cases. J Rheumatol 10:494–495
Hennessy M (1996) Infection of a total knee arthroplasty by Candida parapsilosis. A case report of successful treatment by joint reimplantation with a literature review. Am J Knee Surg 9:133–136
Cushing R, Fulgenzi W (1997) Synovial fluid levels of fluconazole in a patient with Candida parapsilosis prosthetic joint infection who had an excellent clinical response. J Arthroplasty 12:950. https://doi.org/10.1016/S0883-5403(97)90166-2
Fukasawa N, Shirakura K (1997) Candida arthritis after total knee arthroplasty—a case of successful treatment without prosthesis removal. Acta Orthop Scand 68:306–307. https://doi.org/10.3109/17453679708996709
Koch AE (1988) Candida albicans infection of a prosthetic knee replacement: a report and review of the literature. J Rheumatol 15:362–365
Iskander M, Khan M (1988) Candida albicans infection of a prosthetic knee replacement: a case report. J Rheumatol 15:1594–1595
Levine M, Rehm S, Wilde A (1988) Infection with Candida albicans of a total knee arthroplasty. Case report and review of the literature. Clin Orthop Relat Res 235–239
Lambertus M, Thordarson D, Goetz MB (1988) Fungal prosthetic arthritis: presentation of two cases and review of the literature. Rev Infect Dis 10:1038–1043
Darouiche RO, Hamill RJ, Musher DM et al (1989) Periprosthetic candidal infections following arthroplasty. Rev Infect Dis 11:89–96
Paul J, White S, Nicholls K, Crook D (1992) Prosthetic joint infection due to Candida parapsilosis in the UK: case report and literature review. Eur J Clin Microbiol Infect Dis 11:847–849. https://doi.org/10.1007/BF01960889
Tunkel A, Thomas C, Wispelwey B (1993) Candida prosthetic arthritis: report of a case treated with fluconazole and review of the literature. Am J Med 94:100–103. https://doi.org/10.1016/0002-9343(93)90127-B
White A, Goetz M (1995) Candida parapsilosis prosthetic joint infection unresponsive to treatment with fluconazole. Clin Infect Dis 20:1068–1069. https://doi.org/10.1093/CLINIDS/20.4.1068
Simonian P, Brause B, Wickiewicz T (1997) Candida infection after total knee arthroplasty. Management without resection or amphotericin B. J Arthroplasty 12:825–829. https://doi.org/10.1016/S0883-5403(97)90015-2
Selmon G, Slater R, Shepperd J, Wright E (1998) Successful 1-stage exchange total knee arthroplasty for fungal infection. J Arthroplasty 13:114–115. https://doi.org/10.1016/S0883-5403(98)90086-9
Brooks D, Pupparo F (1998) Successful salvage of a primary total knee arthroplasty infected with Candida parapsilosis. J Arthroplasty 13:707–712. https://doi.org/10.1016/S0883-5403(98)80017-X
Wada M, Baba H, Imura S (1998) Prosthetic knee Candida parapsilosis infection. J Arthroplasty 13:479–482. https://doi.org/10.1016/S0883-5403(98)90019-5
Badrul B, Ruslan G (2000) Candida albicans infection of a prosthetic knee replacement: a case report. Med J Malaysia 55(Suppl C):93–96
Yang S, Pao J, Hang Y (2001) Staged reimplantation of total knee arthroplasty after Candida infection. J Arthroplasty 16:529–532. https://doi.org/10.1054/ARTH.2001.21458
Açikgöz Z, Sayli U, Avci S et al (2002) An extremely uncommon infection: Candida glabrata arthritis after total knee arthroplasty. Scand J Infect Dis 34:394–396. https://doi.org/10.1080/00365540110080232
Phelan DM, Osmon DR, Keating MR, Hanssen AD (2002) Delayed reimplantation arthroplasty for candidal prosthetic joint infection: a report of 4 cases and review of the literature. Clin Infect Dis 34:930–938. https://doi.org/10.1086/339212
Wyman J, McGough R, Limbird R (2002) Fungal infection of a total knee prosthesis: successful treatment using articulating cement spacers and staged reimplantation. Orthopedics 25:1391–1394
Lerch K, Kalteis T, Schubert T et al (2003) Prosthetic joint infections with osteomyelitis due to Candida albicans. Mycoses 46:462–466. https://doi.org/10.1046/J.0933-7407.2003.00928.X
Lee G, Kim T, Son J (2012) Primary Candida guilliermondii infection of the knee in a patient without predisposing factors. Case Rep Med. https://doi.org/10.1155/2012/375682
Gaston G, Ogden J (2004) Candida glabrata periprosthetic infection: a case report and literature review. J Arthroplasty 19:927–930. https://doi.org/10.1016/J.ARTH.2004.04.012
Fabry K, Verheyden F, Nelen G (2005) Infection of a total knee prosthesis by Candida glabrata: a case report. Acta Orthop Belg 71:119–121
Dumaine V, Eyrolle L, Baixench M et al (2008) Successful treatment of prosthetic knee Candida glabrata infection with caspofungin combined with flucytosine. Int J Antimicrob Agents 31:398–399. https://doi.org/10.1016/J.IJANTIMICAG.2007.12.001
Bland C, Thomas S (2009) Micafungin plus fluconazole in an infected knee with retained hardware due to Candida albicans. Ann Pharmacother 43:528–531. https://doi.org/10.1345/APH.1L508
Dutronc H, Dauchy FA, Cazanave C et al (2010) Candida prosthetic infections: case series and literature review. Scand J Infect Dis 42:890–895. https://doi.org/10.3109/00365548.2010.498023
Graw B, Woolson S, Huddleston J (2010) Candida infection in total knee arthroplasty with successful reimplantation. J Knee Surg 23:169–174. https://doi.org/10.1055/S-0030-1267470
Wu M, Hsu K (2011) Candidal arthritis in revision knee arthroplasty successfully treated with sequential parenteral-oral fluconazole and amphotericin B-loaded cement spacer. Knee Surg Sports Traumatol Arthrosc 19:273–276. https://doi.org/10.1007/S00167-010-1211-4
Lee Y, Kim H, Lee E et al (2019) Prosthetic Joint Infections caused by Candida species: a systematic review and a case series. Mycopathologia 184:23–33. https://doi.org/10.1007/S11046-018-0286-1
Anagnostakos K, Kelm J, Schmitt E, Jung J (2012) Fungal periprosthetic hip and knee joint infections. J Arthroplasty 27:293–298. https://doi.org/10.1016/j.arth.2011.04.044
Reddy K, Shah J, Kale R, Reddy T (2013) Fungal prosthetic joint infection after total knee arthroplasty. Indian J Orthop 47:526–529. https://doi.org/10.4103/0019-5413.118213
Ueng SWN, Lee C-Y, Hu C et al (2013) What is the success of treatment of hip and knee candidal periprosthetic joint infection? Clin Orthop Relat Res 471:3002–3009. https://doi.org/10.1007/s11999-013-3007-6
Klatte TO, Kendoff D, Kamath AF et al (2014) Single-stage revision for fungal peri-prosthetic joint infection. Bone Joint J 96-B:492–496. https://doi.org/10.1302/0301-620X.96B4.32179
Wiwattanawarang N (2014) Fungal periprosthetic joint infection after total knee arthroplasty. J Med Assoc Thai 97:1358–1363
Wang Q, Shen H, Zhang X et al (2015) Staged reimplantation for the treatment of fungal peri-prosthetic joint infection following primary total knee arthroplasty. Orthop Traumatol Surg Res 101:151–156. https://doi.org/10.1016/J.OTSR.2014.11.014
Jenny J-Y, Goukodadja O, Boeri C, Gaudias J (2016) May one-stage exchange for Candida albicans peri-prosthetic infection be successful? Orthop Traumatol Surg Res 102:127–129. https://doi.org/10.1016/j.otsr.2015.10.001
Ji B, Zhang X, Xu B et al (2017) Single-stage revision for chronic fungal periprosthetic joint infection: an average of 5 years of follow-up. J Arthroplasty 32:2523–2530. https://doi.org/10.1016/j.arth.2017.03.030
Brown TS, Petis SM, Osmon DR et al (2018) Periprosthetic joint infection with fungal pathogens. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.03.003
Koutserimpas C, Samonis G, Velivassakis E et al (2018) Candida glabrata prosthetic joint infection, successfully treated with anidulafungin: a case report and review of the literature. Mycoses 61:266–269. https://doi.org/10.1111/MYC.12736
Kim S-J, Huh J, Odrobina R, Kim JH (2015) Systemic review of published literature on Candida infection following total hip arthroplasty. Mycopathologia 179:173–185. https://doi.org/10.1007/s11046-014-9852-3
Kim J, Lee D, Kang D et al (2018) Efficacy of antifungal-impregnated cement spacer against chronic fungal periprosthetic joint infections after total knee arthroplasty. Knee 25:631–637. https://doi.org/10.1016/J.KNEE.2018.04.004
Gao Z, Li X, Du Y et al (2018) Success rate of fungal peri-prosthetic joint infection treated by 2-stage revision and potential risk factors of treatment failure: a retrospective study. Med Sci Monit 24:5549–5557. https://doi.org/10.12659/MSM.909168
Kuner E, Jöckel J, Orler R, Nüesch R (2019) Periprosthetic knee infection by Mycobacterium bovis and Candida guilliermondii in the context of a zoonosis: a case report and review of the literature. J Med Case Rep. https://doi.org/10.1186/S13256-019-2009-8
Bini Viotti J, Corzo-Pedroza M, Gonzales Zamora J (2019) Prosthetic joint infection caused by Candida lusitaniae: report of a unique case. Acta Clin Belg 74:286–291. https://doi.org/10.1080/17843286.2018.1511264
Oenning S, Moellenbeck B, Gosheger G et al (2020) Fungal periprosthetic knee joint infection in a patient with metamizole-induced agranulocytosis. Arthroplast Today 6:726–730. https://doi.org/10.1016/J.ARTD.2020.07.040
Frieler S, Yilmaz E, Goodmanson R et al (2020) Conversion from knee arthrodesis back to arthroplasty: a particular challenge in combination with fungal periprosthetic joint infection. Arthroplast today 6:1038–1044. https://doi.org/10.1016/J.ARTD.2020.10.007
Saconi E, de Carvalho V, de Oliveira P, Lima A (2020) Prosthetic joint infection due to Candida species: case series and review of literature. Medicine (Baltimore) 99:e19735. https://doi.org/10.1097/MD.0000000000019735
George J, Sainulabdeen J, Chittaranjan S et al (2021) Single-stage revision with fluconazole monotherapy in fungal prosthetic knee joint infections. Arthroplast Today 7:238–241. https://doi.org/10.1016/J.ARTD.2020.12.014
Mafrachi B, Debei A, Muhtaseb F, Al-Ajlouni, JMHammad Y (2021) Fungal prosthetic joint infection following total knee arthroplasty: a case report. J Orthop case reports 11. https://doi.org/10.13107/JOCR.2021.V11.I02.2042
Xin J, Guo Q, Zhang H et al (2020) Candidal periprosthetic joint infection after primary total knee arthroplasty combined with ipsilateral intertrochanteric fracture: a case report. World J Clin cases 8:5401–5408. https://doi.org/10.12998/WJCC.V8.I21.5401
Anagnostakos K, Kelm J, Schmitt E, Jung J (2012) Fungal periprosthetic hip and knee joint infections clinical experience with a 2-stage treatment protocol. J Arthroplasty 27:293–298. https://doi.org/10.1016/j.arth.2011.04.044
Henry MW, Miller AO, Walsh TJ, Brause BD (2017) Fungal musculoskeletal infections. Infect Dis Clin North Am 31:353–368. https://doi.org/10.1016/j.idc.2017.01.006
Tande AJ, Patel R (2014) Prosthetic joint infection. Clin Microbiol Rev 27:302–345. https://doi.org/10.1128/CMR.00111-13
Youssef B, Pavlou G, Tsiridis E (2014) Philadelphia 2013: international consensus meeting on periprosthetic joint infection. HIP Int 24:3–4. https://doi.org/10.5301/hipint.5000127
Pappas P, Kauffman C, Andes D et al (2016) Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 62:e1-50
Fusini F, Aprato A, Massè A et al (2020) Candida periprosthetic infection of the hip: a systematic review of surgical treatments and clinical outcomes. Int Orthop 44:15–22. https://doi.org/10.1007/s00264-019-04369-z
Oussedik SIS, Dodd MB, Haddad FS (2010) Outcomes of revision total hip replacement for infection after grading according to a standard protocol. J Bone Joint Surg Br 92:1222–1226. https://doi.org/10.1302/0301-620X.92B9.23663
Loppini M, Pisano A, Di MM et al (2021) (2021) Outcomes of patients with unexpected diagnosis of infection at total hip or total knee arthroplasty revisions. Int Orthop 1:1–6. https://doi.org/10.1007/S00264-021-05137-8
Madarevic T, Buterin A, Jelicic J et al (2020) (2020) Functional recovery after two-stage short-interval revision of chronic periprosthetic knee joint infection. Int Orthop 454(45):985–989. https://doi.org/10.1007/S00264-020-04566-1
Colò G, Massarini M, Cavagnaro L et al (2020) Exercise therapy indications in metastatic bone patients. Minerva Ortop e Traumatol 71. https://doi.org/10.23736/s0394-3410.19.03960-2
Goss B, Lutton C, Weinrauch P et al (2007) Elution and mechanical properties of antifungal bone cement. J Arthroplasty 22:902–908. https://doi.org/10.1016/j.arth.2006.09.013
Kweon C, McLaren AC, Leon C, McLemore R (2011) Amphotericin B delivery from bone cement increases with porosity but strength decreases. Clin Orthop Relat Res 469:3002–3007. https://doi.org/10.1007/s11999-011-1928-5
Miller RB, McLaren AC, Pauken C et al (2013) Voriconazole is delivered from antifungal-loaded bone cement. Clin Orthop Relat Res 471:195–200. https://doi.org/10.1007/s11999-012-2463-8
Parvizi J (2013) Periprosthetic joint infection: practical management guide. JP Medical Ltd, New Dehli Ltd
Azzam K, Parvizi J, Jungkind D et al (2009) Microbiological, clinical, and surgical features of fungal prosthetic joint infections: a multi-institutional experience. J Bone Jt Surg—Ser A 91:142–149. https://doi.org/10.2106/JBJS.I.00574
Mahmoud SSS, Sukeik M, Alazzawi S et al (2016) Salvage procedures for management of prosthetic joint infection after hip and knee replacements. Open Orthop J 10:600–614. https://doi.org/10.2174/1874325001610010600
Bloom GB, Mears SC, Edwards PK et al (2020) Total knee periprosthetic joint infection in the setting of hematologic malignancy: considerations for management. Arthroplast Today 6:309–315. https://doi.org/10.1016/J.ARTD.2020.04.002
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
FF and SA contributed to the study conception and design. FF, AR, AM, AA, and LS performed literature search; FF, SA, and GC performed the data analysis. FF the first draft of the manuscript was written; LS, SA, GC, and AM revised and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Ethical standards
This article does not contain any studies with human participants or animals performed by any authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Fusini Federico and Colò Gabriele share co-first autorship.
The original online version of this article was revised: The given and family names of authors were interchanged.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fusini, F., Colò, G., Rava, A. et al. Candida periprosthetic infection of the knee: a systematic review of surgical treatments and clinical outcomes. Eur J Orthop Surg Traumatol 33, 899–907 (2023). https://doi.org/10.1007/s00590-022-03224-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03224-z