Abstract
Purpose
Trainee involvement in patient care has raised concerns about the potential risk of adverse outcomes and harming patients. We sought to analyze the impact and potential consequence of surgical trainee involvement in total knee arthroplasty (TKA) procedures in terms of surgical efficacy, patient safety, and functional outcomes.
Methods
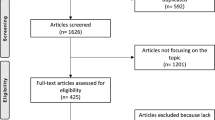
We systematically reviewed Medline/PubMed, EMBASE, the Cochrane library, and Scopus databases in April 2021. Eligible studies reported on the impact of trainee participation in TKA procedures performed with and without such involvement.
Results
Twenty-three publications met our eligibility criteria and were included in our study. These studies reported on 132,624 surgeries completed on 132,416 patients. Specifically, 23,988 and 108,636 TKAs were performed with and without trainee involvement, respectively. The mean operative times for procedures with (n = 19,573) and without (n = 94,581) trainee involvement were 99.77 and 85.05 min, respectively. Both studies that reported data on cost of TKAs indicated a significant increase (p < 0.001) associated with procedures completed by teaching hospitals compared to private practices. Mean overall complication rates were 7.20% and 7.36% for TKAs performed with (n = 9,386) and without (n = 31,406) trainees. Lastly, the mean Knee Society Scale (KSS) knee scores for TKAs with (n = 478) and without (n = 806) trainee involvement were similar; 82.81 and 82.71, respectively.
Conclusion
Our systematic review concurred with previous studies that reported trainee involvement during TKAs increases the mean operative time. However, the overall complication rates and functional outcomes were similar. Larger studies with a better methodology and higher level of evidence are still needed for a resolute conclusion.

Similar content being viewed by others

References
Hoerlesberger N, Glehr M, Amerstorfer F, et al (2020) Residents’ Learning Curve of total knee arthroplasty based on radiological outcome parameters: a retrospective comparative study. J Arthroplasty.
GarrettJr WE (2006) American board of orthopaedic surgery practice of the orthopaedic surgeon: part-II, certification examination case mix. J Bone Jt Surg 88:660
Nilsdotter AK, Toksvig-Larsen S, Roos EM (2009) A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthr Cartil 17:601–606
Steinhaus ME, Christ AB, Cross MB (2017) Total knee arthroplasty for knee osteoarthritis: support for a foregone conclusion? HSS J 13:207–210
Mandl LA (2013) Determining who should be referred for total hip and knee replacements. Nat Rev Rheumatol 9:351–357
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Jt Surg Am 100:1455–1460
Bao MH, Keeney BJ, Moschetti WE et al (2018) Resident participation is not associated with worse outcomes after TKA. Clin Orthop Relat Res 476:1375–1390
Dutta S, Dunnington G, Blanchard MC et al (2003) And doctor, no residents please! J Am Coll Surg 197:1012–1017
Cowles RA, Moyer CA, Sonnad SS et al (2001) Doctor-patient communication in surgery: attitudes and expectations of general surgery patients about the involvement and education of surgical residents. J Am Coll Surg 193:73–80
Schoenfeld AJ, Serrano JA, Waterman BR et al (2013) The impact of resident involvement on post-operative morbidity and mortality following orthopaedic procedures: a study of 43,343 cases. Arch Orthop Trauma Surg 133:1483–1491
ACGME (2014) Orthopaedic surgery minimum numbers: review committeee for orthopaedic surgery. http://www.acgme.org/portals/0/pfassets/programresources/260_ors_case_log_minimum_numbers.pdf. Accessed 9 Dec 2020
Beattie N, Maempel JF, Roberts S et al (2018) Surgery performed by supervised registrars does not adversely affect medium-term functional outcomes after total knee replacement. Ann R Coll Surg Engl 100:57–62
Weber M, Worlicek M, Voellner F et al (2018) Surgical training does not affect operative time and outcome in total knee arthroplasty. PLoS ONE 13:e0197850
Perfetti DC, Sodhi N, Khlopas A et al (2017) Is Orthopaedic department teaching status associated with adverse outcomes of primary total knee arthroplasty? Surg Technol Int 31:379–383
Woolson ST, Kang MN (2007) A comparison of the results of total hip and knee arthroplasty performed on a teaching service or a private practice service. J Bone Jt Surg Am 89:601–607
Wilson T, Sahu A, Johnson DS, Turner PG (2010) The effect of trainee involvement on procedure and list times: a statistical analysis with discussion of current issues affecting orthopaedic training in UK. Surgeon 8:15–19
Storey R, Frampton C, Kieser D et al (2018) Does orthopaedic training compromise the outcome in knee joint arthroplasty? J Surg Educ 75:1292–1298
Schnurr C, Eysel P, König DP (2011) Do residents perform TKAs using computer navigation as accurately as consultants? Orthopedics 34:174
Bohl DD, Fu MC, Golinvaux NS et al (2014) The “July effect” in primary total hip and knee arthroplasty: analysis of 21,434 cases from the ACS-NSQIP database. J Arthroplast 29:1332–1338
Kazarian GS, Lawrie CM, Barrack TN et al (2019) The impact of surgeon volume and training status on implant alignment in total knee arthroplasty. J Bone Jt Surg Am 101:1713–1723
Khakha RS, Chowdhry M, Sivaprakasam M et al (2015) Radiological and functional outcomes in computer assisted total knee arthroplasty between consultants and trainees—a prospective randomized controlled trial. J Arthroplast 30:1344–1347
Haughom BD, Schairer WW, Hellman MD et al (2014) Does resident involvement impact post-operative complications following primary total knee arthroplasty? An analysis of 24,529 cases. J Arthroplast 29:1468-1472.e2
Lavernia CJ, Sierra RJ, Hernandez RA (2000) The cost of teaching total knee arthroplasty surgery to orthopaedic surgery residents. Clin Orthop Relat Res 99–107
Theelen L, Bischoff C, Grimm B, Heyligers IC (2018) Current practice of orthopaedic surgical skills training raises performance of supervised residents in total knee arthroplasty to levels equal to those of orthopaedic surgeons. Perspect Med Educ 7:126–132
Insall J, Dorr L, Scott R, Scott W (1989) Rationale of the Knee Society clincal rating system. Clin Orthop Relat Res 13–14
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69
Davies A (2002) Rating systems for total knee replacement. Knee 9:261–266
Ware J Jr, Sherbourne C (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Gromov K, Korchi M, Thomsen M et al (2014) What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop 85:480–487
Kim Y, Park J, Kim J, Park S (2014) The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 38:379–385
Ritter M, Davis K, Meding J et al (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93:1588–1596
Goto K, Katsuragawa Y, Miyamoto Y (2020) Outcomes and component-positioning in total knee arthroplasty may be comparable between supervised trained surgeons and their supervisor. Knee Surg Relat Res 32:1–6
Khanuja HS, Solano MA, Sterling RS et al (2019) Surgeon mean operative times in total knee arthroplasty in a variety of settings in a health system. J Arthroplasty 34:2569–2572
Pugely AJ, Gao Y, Martin CT et al (2014) The effect of resident participation on short-term outcomes after orthopaedic surgery. Clin Orthop Relat Res 472:2290–2300
Gandhi R, Tso P, Davis A, Mahomed NN (2009) Outcomes of total joint arthroplasty in academic versus community hospitals. Can J Surg 52:413–416
Faulkner A, Reidy M, Davies P et al (2018) Balancing training and outcomes in total knee replacement: a ten-year review. Surgeon 16:227–231
Wilson M, Dowsey M, Spelman T, Choong P (2016) Impact of surgical experience on outcomes in total joint arthroplasties. ANZ J Surg 86:967–972
Bottomley N, Jones L, Rout R et al (2016) A survival analysis of 1084 knees of the Oxford unicompartmental knee arthroplasty: a comparison between consultant and trainee surgeons. Bone Jt J 98-B:22–27
Rana A, Bozic K (2015) Bundled payments in orthopaedics. Clin Orthop Relat Res 473:422–425
Ahmed N, Devitt K, Keshet I et al (2014) A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg 259:1041–1053
Antiel R, Reed D, Van Arendonk K et al (2013) Effects of duty hour restrictions on core competencies, education, quality of life, and burnout among general surgery interns. JAMA Surg 148:448–455
Holt G, Nunn T, Gregori A (2008) Ethical dilemmas in orthopaedic surgical training. J Bone Joint Surg Am 90:2798–2803
Pour AE, Bradbury TL, Horst P et al (2016) Trends in primary and revision knee arthroplasty among orthopaedic surgeons who take the American Board of Orthopaedics part II exam. Int Orthop 40:2061–2067
Greenwald AS, Bassano A, Wiggins S, Froimson MI (2016) Alternative reimbursement models: bundled payment and beyond: AOA critical issues. J Bone Joint Surg Am 98:e45
Babineau TJ, Becker J, Gibbons G et al (2004) The “Cost” of operative training for surgical residents. Arch Surg 139:366–370
Edelstein AI, Lovecchio FC, Saha S et al (2014) Impact of resident involvement on orthopaedic surgery outcomes: an analysis of 30,628 patients from the American college of surgeons national surgical quality improvement program database. J Bone Jt Surg Am 96:e131
Anderson KL, Koval KJ, Spratt KF (2009) Hip fracture outcome: is there a “July effect”? Am J Orthop (Belle Mead NJ) 38:606–611
Advani V, Ahad S, Gonczy C et al (2012) Does resident involvement effect surgical times and complication rates during laparoscopic appendectomy for uncomplicated appendicitis? An analysis of 16,849 cases from the ACS-NSQIP. Am J Surg 203:347–352
Hernández-Irizarry R, Zendejas B, Ali S et al (2012) Impact of resident participation on laparoscopic inguinal hernia repairs: are residents slowing us down? J Surg Educ 69:746–752
Davis S, Husain F, Lin E et al (2013) Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg 216:96–104
Song K, Pan P, Yao Y et al (2019) The incidence and risk factors for allogenic blood transfusion in total knee and hip arthroplasty. J Orthop Surg Res 14:1–6
Menendez ME, Lu N, Huybrechts KF et al (2016) Variation in use of blood transfusion in primary total hip and knee arthroplasties. J Arthroplasty 31:2757-2763.e2
Lu Q, Peng H, Zhou GJ, Yin D (2018) Perioperative blood management strategies for total knee arthroplasty. Orthop Surg 10:8–16
Baek H, Cho M, Kim S, et al (2018) Analysis of length of hospital stay using electronic health records: A statistical and data mining approach. PLoS One 13
Rotter T, Kinsman L, James E, et al (2010) Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev
Urish KL, Qin Y, Salka B et al (2020) Comparison of readmission and early revision rates as a quality metric in total knee arthroplasty using the nationwide readmission database. Ann Transl Med 8:687–687
Manley M, Ong K, Lau E, Kurtz S (2009) Total knee arthroplasty survivorship in the United States medicare population: effect of hospital and surgeon procedure volume. J Arthroplast 24:1061–1067
Koh C, Zeng I, Ravi S et al (2017) Periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11,134 knees. Clin Orthop Relat Res 475:2194–2201
Rissman C, Keeney B, Ercolano E, Koenig K (2016) Predictors of facility discharge, range of motion, and patient-reported physical function improvement after primary total knee arthroplasty: a prospective cohort analysis. J Arthroplast 31:36–41
Barsoum WK, Murray TG, Klika AK et al (2010) Predicting patient discharge disposition after total joint arthroplasty in the United States. J Arthroplasty 25:885–892
Bozic KJ, Wagie A, Naessens JM et al (2006) Predictors of discharge to an inpatient extended care facility after total hip or knee arthroplasty. J Arthroplasty 21:151–156
Laubenthal K, Smidt G, Kettelkamp D (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52:34–43
Rowe P, Myles C, Walker C, Nutton R (2000) Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture 12:143–155
Fang D, Ritter M, Davis K (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 24:39–43
Tew M, Waugh W (1985) Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br 67:551–556
Madanipour S, Singh P, Karia M et al (2021) Trainee performed total knee arthroplasty is safe and effective: a systematic review and meta-analysis comparing outcomes between trainees and consultants. Knee 30:291–304
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
RM, NVS, QN, and AVM all have no financial disclosures to report. AVM is a board or committee member of the Musculoskeletal Tumor Society, and an editorial or governing board member of the World Journal of Orthopedics, outside the submitted work. QN reports editorial or governing board membership of the European Journal of Orthopaedic Surgery and Traumatology
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marder, R.S., Shah, N.V., Naziri, Q. et al. The impact of surgical trainee involvement in total knee arthroplasty: a systematic review of surgical efficacy, patient safety, and outcomes. Eur J Orthop Surg Traumatol 33, 255–298 (2023). https://doi.org/10.1007/s00590-021-03179-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03179-7