Abstract
Purpose
Opioids have long been a mainstay of treatment for pain in patients with orthopaedic injuries, but little is known about the accuracy of self-reported narcotic usage in orthopaedic trauma. The purpose of this study is to evaluate the accuracy of self-reported opioid usage in orthopaedic trauma patients.
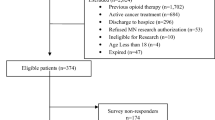
Methods
A retrospective review of all new patients presenting to the orthopaedic trauma clinic of a level 1 trauma centre with a chief complaint of recent orthopaedic-related injury over a 2-year time frame was conducted. Participants were administered a survey inquiring about narcotic usage within the prior 3 months. Responses were cross-referenced against a query of a statewide prescription drug monitoring program system.
Results
The study comprised 241 participants; 206 (85.5%) were accurate reporters, while 35 (14.5%) were inaccurate reporters. Significantly increased accuracy was associated with hospital admission prior to clinic visit (β = − 1.33; χ2 = 10.68, P < 0.01; OR: 0.07, 95% CI 0.01–0.62). Decreased accuracy was associated with higher pre-visit total morphine equivalent dose (MED) (β = 0.002; χ2 = 11.30, P < 0.01), with accurate reporters having significantly lower pre-index visit MED levels compared to underreporters (89.2 ± 208.7 mg vs. 249.6 ± 509.3 mg; P = 0.04). An Emergency Department (ED) visit prior to the index visit significantly predicted underreporting (β = 0.424; χ2 = 4.28, P = 0.04; OR: 2.34, 95% CI 1.01–5.38).
Conclusion
This study suggests that most new patients presenting to an orthopaedic trauma clinic with acute injury will accurately report their narcotic usage within the preceding 3 months. Prior hospital admissions increased the likelihood of accurate reporting while higher MEDs or an ED visit prior to the initial visit increased the likelihood of underreporting.
Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are available from the corresponding author (J.G.L.) upon reasonable request.
References
Kuehn BM (2021) Massive costs of the US opioid epidemic in lives and dollars. JAMA 325:2040. https://doi.org/10.1001/jama.2021.7464
Jain N, Brock JL, Phillips FM et al (2018) Chronic preoperative opioid use is a risk factor for increased complications, resource use, and costs after cervical fusion. Spine J 18:1989–1998. https://doi.org/10.1016/j.spinee.2018.03.015
Morris BJ, Sciascia AD, Jacobs CA, Edwards TB (2016) Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elb Surg 25:619–623. https://doi.org/10.1016/j.jse.2015.09.017
Raad M, Jain A, Neuman BJ et al (2018) Association of patient-reported narcotic use with short- and long-term outcomes after adult spinal deformity surgery: multicenter study of 425 patients with 2-year follow-up. Spine (Phila Pa 1976) 43:1340–1346. https://doi.org/10.1097/BRS.0000000000002631
Smith SR, Bido J, Collins JE et al (2017) Impact of preoperative opioid use on total knee arthroplasty outcomes. J Bone Joint Surg Am 99:803–808. https://doi.org/10.2106/JBJS.16.01200
Ben-Ari A, Chansky H, Rozet I (2017) Preoperative opioid use is associated with early revision after total knee arthroplasty: a study of male patients treated in the veterans affairs system. J Bone Joint Surg Am 99:1–9. https://doi.org/10.2106/JBJS.16.00167
Parker Vail T (2011) Preoperative pain management decisions impact outcome after total knee arthroplasty-implications for opiate use: commentary on an article by Michael G. Zywiel, MD, et al.: “Chronic opioid use prior to total knee arthroplasty.” J Bone Joint Surg Am 93:e1291–e1301. https://doi.org/10.2106/JBJS.K.01145
Nguyen L-CL, Sing DC, Bozic KJ (2016) Preoperative reduction of opioid use before total joint arthroplasty. J Arthroplasty 31:282–287. https://doi.org/10.1016/j.arth.2016.01.068
Moyo P, Simoni-Wastila L, Griffin BA et al (2017) Impact of prescription drug monitoring programs (PDMPs) on opioid utilization among Medicare beneficiaries in 10 US States. Addiction 112:1784–1796. https://doi.org/10.1111/add.13860
Suffoletto B, Lynch M, Pacella CB et al (2018) The effect of a statewide mandatory prescription drug monitoring program on opioid prescribing by emergency medicine providers across 15 hospitals in a single health system. J Pain 19:430–438. https://doi.org/10.1016/j.jpain.2017.11.010
Hawk K, D’Onofrio G, Fiellin DA et al (2018) Past-year prescription drug monitoring program opioid prescriptions and self-reported opioid use in an emergency department population with opioid use disorder. Acad Emerg Med 25:508–516. https://doi.org/10.1111/acem.13352
Wilson MP, Cucciare MA, Porter A et al (2019) The utility of a statewide prescription drug-monitoring database vs the Current Opioid Misuse Measure for identifying drug-aberrant behaviors in emergency department patients already on opioids. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2019.05.035
Hereford TE, Cryar KA, Edwards PK et al (2018) Patients with hip or knee arthritis underreport narcotic usage. J Arthroplasty 33:3113–3117. https://doi.org/10.1016/j.arth.2018.05.032
Ahn J, Bohl DD, Tabaraee E et al (2016) Preoperative narcotic utilization: accuracy of patient self-reporting and its association with postoperative narcotic consumption. J Neurosurg Spine 24:206–214. https://doi.org/10.3171/2015.3.SPINE141300
Crawford DA, Andrews RL, Hurst JM et al (2020) Accuracy of patient-reported preoperative opioid use and impact on continued opioid use after outpatient arthroplasty. J Arthroplasty 35:1504–1507. https://doi.org/10.1016/j.arth.2020.01.064
van Boekel LC, Brouwers EPM, van Weeghel J, Garretsen HFL (2013) Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend 131:23–35. https://doi.org/10.1016/j.drugalcdep.2013.02.018
Bicket MC, Long JJ, Pronovost PJ et al (2017) Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg 152:1066–1071. https://doi.org/10.1001/jamasurg.2017.0831
Davis TC, Wolf MS, Bass PF 3rd et al (2006) Low literacy impairs comprehension of prescription drug warning labels. J Gen Intern Med 21:847–851. https://doi.org/10.1111/j.1525-1497.2006.00529.x
Hoppe JA, Nelson LS, Perrone J, Weiner SG (2015) Opioid prescribing in a cross section of US Emergency Departments. Ann Emerg Med 66:253-259.e1. https://doi.org/10.1016/j.annemergmed.2015.03.026
Gwadry-Sridhar FH, Arnold JMO, Zhang Y et al (2005) Pilot study to determine the impact of a multidisciplinary educational intervention in patients hospitalized with heart failure. Am Heart J 150:982. https://doi.org/10.1016/j.ahj.2005.08.016
Blinder D, Rotenberg L, Peleg M, Taicher S (2001) Patient compliance to instructions after oral surgical procedures. Int J Oral Maxillofac Surg 30:216–219. https://doi.org/10.1054/ijom.2000.0045
Kharod BV, Johnson PB, Nesti HA, Rhee DJ (2006) Effect of written instructions on accuracy of self-reporting medication regimen in glaucoma patients. J Glaucoma 15:244–247. https://doi.org/10.1097/01.ijg.0000212213.18018.8f
Ives TJ, Chelminski PR, Hammett-Stabler CA et al (2006) Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Serv Res 6:46. https://doi.org/10.1186/1472-6963-6-46
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors were involved in the study design, collection of data, manuscript preparation, and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
This study was approved by our institutional review board. Due to the retrospective nature of this work, a waiver of informed consent was granted. This study was approved by the relevant institutional ethical board and was in full compliance with the Declaration of Helsinki and its appendages.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hijji, F.Y., Sanda, T., Huff, S.D. et al. Accuracy of self-reported opioid use in orthopaedic trauma patients. Eur J Orthop Surg Traumatol 33, 185–190 (2023). https://doi.org/10.1007/s00590-021-03178-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03178-8