Abstract
Purpose
Hyperextension after total knee arthroplasty (TKA) is related to worse functional outcomes. Among the reported predictive factors, it is unclear whether prosthesis design affects postoperative hyperextension. Hence, our objectives were to (1) compare time-dependent changes of the extension angle following multi-radius (MR) and single-radius (SR) TKA and (2) assess predictive factors for the hyperextension.
Methods
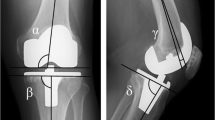
In this study, consecutive 136 MR TKAs and consecutive 71 SR TKAs performed by a single surgeon were reviewed. The extension angle was evaluated by digitized full-extension lateral radiographs at preoperative, 3 months and at 1 and 2 years after TKA. A positive value was defined as hyperextension. A multiple regression analysis was used to determine predictive factors for the extension angle and the risk of hyperextension > 5°.
Results
The postoperative extension angle of both groups gradually increased during the first 2 years and the SR group finally progressed with 4.04° greater extension than the MR group (p < 0.01). The incidence of hyperextension > 5° in the SR group was 18.3% and for the MR group, 7.4% (p = 0.02). However, the Oxford knee scores was nonsignificant different between the groups (p = 0.15). Preoperative extension angle, sagittal femoral component angle (SFA) and SR prosthesis were predictive factors for the extension angle at 2 years after TKA and were also associated with hyperextension > 5°.
Conclusions
The extension angle of the SR group became significantly more extended than that of the MR group during the first two years after TKA. Hence, ideal extension position immediately after SR TKA may be different from that of the MR TKA prosthesis. The preoperative extension angle, SFA and SR prosthesis were factors that were associated with postoperative hyperextension.




Similar content being viewed by others
References
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 7 93(17):1588–96
Collier MB, Engh CA Jr, McAuley JP, Engh GA (2007) Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg Am 89(6):1306–1314
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R et al (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Ritter MA, Lutgring JD, Davis KE, Berend ME, Pierson JL, Meneghini RM (2007) The role of flexion contracture on outcomes in primary total knee arthroplasty. J Arthroplast 22(8):1092–1096
Kim SH, Ro DH, Cho Y, Lee YM, Lee S, Lee MC (2017) What is the ideal degree of extension after primary total knee arthroplasty? J Arthroplast 32(9):2717–2724
Lee HJ, Park YB, Lee DH, Kim KH, Ham DW, Kim SH (2019) Risk factors of hyperextension and its relationship with the clinical outcomes following mobile-bearing total knee arthroplasty. Arch Orthop Trauma Surg 139(9):1293–1305
Lee SS, Kim JH, Heo JW, Moon YW (2019) Gradual change in knee extension following total knee arthroplasty using ultracongruent inserts. Knee 26(4):905–913
Siddiqui MM, Yeo SJ, Sivaiah P, Chia SL, Chin PL, Lo NN (2012) Function and quality of life in patients with recurvatum deformity after primary total knee arthroplasty: a review of our joint registry. J Arthroplast 27(6):1106–1110
Parratte S, Pagnano MW (2008) Instability after total knee arthroplasty. J Bone Joint Surg Am 90(1):184–194
Ritter MA, Lutgring JD, Davis KE, Berend ME (2008) The effect of postoperative range of motion on functional activities after posterior cruciate-retaining total knee arthroplasty. J Bone Joint Surg Am 90(4):777–784
Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME (2001) Total knee replacement in patients with genu recurvatum. Clin Orthop Relat Res 393:244–249
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Mizu-Uchi H, Hamai S et al (2014) Extension gap needs more than 1-mm laxity after implantation to avoid postoperative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(12):3174–3180
Frankel VH, Burstein AH, Brooks DB (1971) Biomechanics of internal derangement of the knee. Pathomechanics as determined by analysis of the instant centers of motion. J Bone Joint Surg Am 53(5):945–62
Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG (1993) The axes of rotation of the knee. Clin Orthop Relat Res 290:259–268 (PMID: 8472457)
Asano T, Akagi M, Nakamura T (2005) The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image-matching technique. J Arthroplasty 20(8):1060–1067
Stoddard JE, Deehan DJ, Bull AM, McCaskie AW, Amis AA (2013) The kinematics and stability of single-radius versus multi-radius femoral components related to mid-range instability after TKA. J Orthop Res 31(1):53–58
Liu S, Long H, Zhang Y, Ma B, Li Z (2016) Meta-analysis of outcomes of a single-radius versus multi-radius femoral design in total knee arthroplasty. J Arthroplasty 31(3):646–654
Luo Z, Luo Z, Wang H, Xiao Q, Pei F, Zhou Z (2019) Long-term results of total knee arthroplasty with single-radius versus multi-radius posterior-stabilized prostheses. J Orthop Surg Res 16 14(1):139
Hinarejos P, Puig-Verdie L, Leal J, Pelfort X, Torres-Claramunt R, Sánchez-Soler J, Monllau JC (2016) No differences in functional results and quality of life after single-radius or multiradius TKA. Knee Surg Sports Traumatol Arthrosc 24(8):2634–2640
Chotanaphuti T, Panichcharoen W, Laoruengthana A (2012) Comparative study of anatomical landmark technique and self-aligned tibial component rotation determined by computer-assisted TKA. J Med Assoc Thai 95(Suppl 10):S37-41
Scuderi GR, Kochhar T (2007) Management of flexion contracture in total knee arthroplasty. J Arthroplast 22(4 Suppl 1):20–24
Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME (2003) Genu recurvatum in total knee replacement. Clin Orthop Relat Res 416:64–67
Laoruengthana A, Rattanaprichavej P, Mahatthanatrakul A, Tantimethanon T, Lohitnavy M, Pongpirul K (2020) Periarticular injection of ketorolac augmenting intravenous administration of ketorolac for postoperative pain control: a randomized controlled trial in simultaneous bilateral total knee arthroplasty. J Knee Surg. https://doi.org/10.1055/s-0040-1721088 (Epub ahead of print PMID: 33231281)
Khalifa AA, Mullaji AB, Mostafa AM, Farouk OA (2021) A protocol to systematic radiographic assessment of primary total knee arthroplasty. Orthop Res Rev 17(13):95–106. https://doi.org/10.2147/ORR.S320372.PMID:34305412;PMCID:PMC8294812
Gromov K, Korchi M, Thomsen MG, Husted H, Troelsen A (2014) What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop 85(5):480–487
Larsen B, Jacofsky MC, Jacofsky DJ (2015) Quantitative, comparative assessment of gait between single-radius and multi-radius total knee arthroplasty designs. J Arthroplasty 30(6):1062–1067
Sumner B, McCamley JD, Jacofsky DJ, Jacofsky MC (2019) Comparison of knee kinematics and kinetics during stair ascent in single-radius and multiradius total knee arthroplasty. J Knee Surg 32(9):872–878
Kim DH, Kim DK, Lee SH, Kim KI, Bae DK (2015) Is single-radius design better for quadriceps recovery in total knee arthroplasty? Knee Surg Relat Res 27(4):240–6. https://doi.org/10.5792/ksrr.2015.27.4.240 (Epub 2015 Dec 1 PMID: 26676282; PMCID: PMC4678245)
Mortazavi SMJ, Razzaghof M, Noori A, Okati A (2020) Late-Onset De Novo Genu Recurvatum after Primary Total Knee Arthroplasty: A Potential Indication for Isolated Polyethylene Exchange. Arthroplast Today 13 6(3):492–495
Krackow KA, Weiss AP (1990) Recurvatum deformity complicating performance of total knee arthroplasty. A brief note. J Bone Joint Surg Am 72(2):268–71 (PMID: 2303513)
Hamai S, Miura H, Matsuda S, Shimoto T, Higaki H, Iwamoto Y (2010) Contact stress at the anterior aspect of the tibial post in posterior-stabilized total knee replacement. J Bone Joint Surg Am 21, 92(8):1765–73. https://doi.org/10.2106/JBJS.I.00479. Erratum in: J Bone Joint Surg Am. 2010 Sep 15;92(12):2210. PMID: 20660240.
Duenes M, Schoof L, Schwarzkopf R, Meftah M (2020) Complex regional pain syndrome following total knee arthroplasty. Orthopedics 1 43(6):e486–e491. https://doi.org/10.3928/01477447-20200923-05 (Epub 2020 Oct 1 PMID: 33002178)
Royeca JM, Cunningham CM, Pandit H, King SW (2019) Complex regional pain syndrome as a result of total knee arthroplasty: A case report and review of literature. Case Rep Womens Health 24(23):e00136. https://doi.org/10.1016/j.crwh.2019.e00136 (PMID:31388503 PMCID:PMC6675945)
Burns AW, Parker DA, Coolican MR, Rajaratnam K (2006) Complex regional pain syndrome complicating total knee arthroplasty. J Orthop Surg (Hong Kong) 14(3):280–283. https://doi.org/10.1177/230949900601400309 (PMID: 17200529)
Laoruengthana A, Rattanaprichavej P, Tantimethanon T, Eiamjumras W, Teekaweerakit P, Pongpirul K (2021) Usefulness of an accelerometer-based navigation system in bilateral one-stage total knee arthroplasty. BMC Musculoskelet Disord 10 22(1):164
Zhao L, Xu F, Lao S, Zhao J, Wei Q (2020) Comparison of the clinical effects of computer-assisted and traditional techniques in bilateral total knee arthroplasty: A meta-analysis of randomized controlled trials. PLoS One 25 15(9):e0239341
Kim JS, Cho CH, Lee MC, Han HS (2021) Risk factors of de novo hyperextension developed after posterior cruciate ligament substituting total knee arthroplasty: a matched case-control study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06618-4 (Epub ahead of print. PMID: 34028564)
Acknowledgements
We thank Mr. Roy I. Morien of the Naresuan University Graduate School for his assistance in editing the English expression and grammar in this document. We also thank Pariphat Chompoonutprapa, MD, Watcharapong Eiamjumras, MD, Thanawat Tantimethanon, MD, Parin Samapath, MD, for their technical assistance.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
AL contributed to the conception and design of the study, as well as surgeons who performed the operation. PR and AL wrote and completed the manuscript. PR, PS, MG and PT collected the required data. AL, PR and KP was responsible for data interpretation and performed the statistical analysis. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
This study was approved by the appropriate Naresuan University Institutional Review Board. This study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Laoruengthana, A., Rattanaprichavej, P., Suangyanon, P. et al. Hyperextension following two different designs of fixed-bearing posterior-stabilized total knee arthroplasty. Eur J Orthop Surg Traumatol 32, 1641–1650 (2022). https://doi.org/10.1007/s00590-021-03150-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03150-6