Abstract
Purpose
The purpose of this study is to determine the effects of blood transfusion timing in hip fracture patients.
Methods
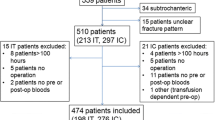
A consecutive series of hip fracture patients 55 years and older who required a blood transfusion during hospitalization were reviewed for demographic, injury, clinical outcome, and cost information. A validated risk predictive score (STTGMA) was calculated for each patient. Patients were stratified to preoperative, intraoperative, or postoperative first transfusion cohorts. The intraoperative and postoperative cohorts were matched by STTGMA, sex, and procedure to the preoperative cohort. Baseline patient characteristics and outcomes were compared before and after matching.
Results
Prior to matching, the preoperative cohort was more often male (p < 0.001) with increased Charlson comorbidity index (p = 0.012), ASA class (p < 0.002), STTGMA (p < 0.001), total transfused volume (p = 0.002), incidence of inpatient mortality (p = 0.045), myocardial infarction (p = 0.005) and cardiac arrest (p = 0.014). After matching, the preoperative cohort had increased total transfused volume (p = 0.015) and decreased pneumonia incidence (p = 0.040).
Conclusion
Matching STTGMA score, sex, and procedure results in non-inferior outcomes among hip fracture patients receiving preoperative first blood transfusions compared to intraoperative and postoperative transfusions.
Similar content being viewed by others
References
Brauer CA, Coca-Perraillon M, Cutler DM et al (2009) Incidence and mortality of hip fractures in the United States. JAMA 302(14):1573–1579. https://doi.org/10.1001/jama.2009.1462
Downey C, Kelly M, Quinlan JF (2019) Changing trends in the mortality rate at 1-year post hip fracture—a systematic review. World J Orthop 10(3):166–175. https://doi.org/10.5312/wjo.v10.i3.166
Endo A, Baer HJ, Nagao M et al (2018) Prediction model of in-hospital mortality after hip fracture surgery. J Orthop Trauma 32(1):34–38. https://doi.org/10.1097/BOT.0000000000001026
Sheehan KJ, Guerrero EM, Tainter D et al (2019) Prognostic factors of in-hospital complications after hip fracture surgery: a scoping review. Osteoporos Int 30(7):1339–1351. https://doi.org/10.1007/s00198-019-04976-x
Carpintero P, Caeiro JR, Carpintero R et al (2014) Complications of hip fractures: a review. World J Orthop 5(4):402–411. https://doi.org/10.5312/wjo.v5.i4.402
Sim YE, Sim SD, Seng C et al (2018) preoperative anemia, functional outcomes, and quality of life after hip fracture surgery. J Am Geriatr Soc 66(8):1524–1531. https://doi.org/10.1111/jgs.15428
Carson JL, Terrin ML, Noveck H et al (2011) Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 365(26):2453–2462. https://doi.org/10.1056/NEJMoa1012452
Parker MJ (2013) Randomised trial of blood transfusion versus a restrictive transfusion policy after hip fracture surgery. Injury 44(12):1916–1918. https://doi.org/10.1016/j.injury.2013.04.033
Mao T, Gao F, Han J et al (2017) Restrictive versus liberal transfusion strategies for red blood cell transfusion after hip or knee surgery: A systematic review and meta-analysis. Medicine (Baltimore) 96(25):e7326. https://doi.org/10.1097/MD.0000000000007326
Mueller MM, Van Remoortel H, Meybohm P et al (2019) Patient blood management: recommendations from the 2018 Frankfurt consensus conference. JAMA 321(10):983–997. https://doi.org/10.1001/jama.2019.0554
Müller S, Oberle D, Drechsel-Bäuerle U et al (2018) Mortality, morbidity and related outcomes following perioperative blood transfusion in patients with major orthopaedic surgery: a systematic review. Transfus Med Hemotherapy 45(5):355–367. https://doi.org/10.1159/000481994
Leuzinger E, Poblete B, Konrad CJ et al (2018) How current transfusion practices in geriatric patients with hip fracture still differ from current guidelines and the effects on outcome: a retrospective observational study. Eur J Anaesthesiol 35(12):972–979. https://doi.org/10.1097/EJA.0000000000000883
Arshi A, Lai WC, Iglesias BC et al (2021) Blood transfusion rates and predictors following geriatric hip fracture surgery. HIP Int 31:272–279. https://doi.org/10.1177/1120700019897878
Smeets SJM, Verbruggen JPAM, Poeze M (2018) Effect of blood transfusion on survival after hip fracture surgery. Eur J Orthop Surg Traumatol 28(7):1297–1303. https://doi.org/10.1007/s00590-018-2205-z
Wang C, Kou H, Li X, et al. Association Between Preoperative Blood Transfusion and Postoperative Venous Thromboembolism: Review Meta-Analysis. Ann Vasc Surg. https://doi.org/10.1016/j.avsg.2020.11.033
Mehta VA, Van Belleghem F, Price M et al (2021) Hematocrit as a predictor of preoperative transfusion-associated complications in spine surgery: a NSQIP study. Clin Neurol Neurosurg 200:106322. https://doi.org/10.1016/j.clineuro.2020.106322
Papageorge CM, Kennedy GD, Carchman EH (2017) Preoperative blood transfusion is a predictor of worse short-term postoperative outcomes after colectomy. Surgery 161(4):1067–1075. https://doi.org/10.1016/j.surg.2016.08.042
Meinberg EG, Agel J, Roberts CS et al (2018) Fracture and ZPENDIUM-2018. J Orthop Trauma 32(Suppl 1):S1–S170. https://doi.org/10.1097/BOT.0000000000001063
Konda SR, Seymour R, Manoli A et al (2016) Development of a Middle-Age and Geriatric Trauma Mortality Risk Score A Tool to Guide Palliative Care Consultations. Bull Hosp Jt Dis 2013. 74(4):298–305
Ho DE, Imai K, King G et al (2011) MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw 42(8):1–28
R Core Team. R (2020) A language and environment for statistical computing. R Found Stat Comput. https://www.R-project.org/
Brunskill SJ, Millette SL, Shokoohi A, et al 2015 Red blood cell transfusion for people undergoing hip fracture surgery. Cochrane Database Syst Rev.(4):CD009699. https://doi.org/10.1002/14651858.CD009699.pub2
Konda SR, Johnson JR, Kelly EA et al (2020) Can we accurately predict which geriatric and middle-aged hip fracture patients will experience a delay to surgery? Geriatr Orthop Surg Rehabil 11:2151459320946021. https://doi.org/10.1177/2151459320946021
Konda SR, Lott A, Egol KA (2018) The coming hip and femur fracture bundle: a new inpatient risk stratification tool for care providers. Geriatr Orthop Surg Rehabil 9:2151459318795311. https://doi.org/10.1177/2151459318795311
Konda SR, Lott A, Egol KA (2020) Development of a value-based algorithm for inpatient triage of elderly hip fracture patients. J Am Acad Orthop Surg 28(13):e566–e572. https://doi.org/10.5435/JAAOS-D-18-00400
Konda SR, Lott A, Saleh H et al (2019) Using trauma triage score to risk-stratify inpatient triage, hospital quality measures, and cost in middle-aged and geriatric orthopaedic trauma patients. J Orthop Trauma 33(10):525–530. https://doi.org/10.1097/BOT.0000000000001561
Konda SR, Ranson RA, Solasz SJ et al (2020) Modification of a validated risk stratification tool to characterize geriatric hip fracture outcomes and optimize care in a post-COVID-19 world. J Orthop Trauma 34(9):e317–e324. https://doi.org/10.1097/BOT.0000000000001895
Konda SR, Saleh H, Lott A et al (2018) Predicting discharge location among low-energy hip fracture patients using the score for trauma triage in the geriatric and middle-aged (STTGMA). Adv Orthop 2018:9793435. https://doi.org/10.1155/2018/9793435
Konda SR, Parola R, Perskin C et al (2021) ASA physical status classification improves predictive ability of a validated trauma risk score. Geriatr Orthop Surg Rehabil 12:2151459321989534. https://doi.org/10.1177/2151459321989534
Konda SR, Dedhia N, Rettig SA, et al. “Damage Control” fixation of displaced femoral neck fractures in high-risk elderly patients: a feasibility case series. J Orthop Trauma. Accepted for publication, not yet published.
Ekström W, Samuelsson B, Ponzer S et al (2015) Sex effects on short-term complications after hip fracture: a prospective cohort study. Clin Interv Aging 10:1259–1266. https://doi.org/10.2147/CIA.S80100
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The study was approved by the NYU Grossman School of Medicine Institutional Review Board, New York, NY. The IRB Number is i20-01766.
Informed consent
A Waiver of Consent was approved by the NYU Grossman School of Medicine Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parola, R., Konda, S.R., Perskin, C.R. et al. Transfusion timing relative to surgery does not impact outcomes in hip fracture patients. Eur J Orthop Surg Traumatol 32, 725–732 (2022). https://doi.org/10.1007/s00590-021-03033-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03033-w