Abstract
Background
Excessive opioid prescriptions after orthopedic surgery are common. The purpose of this study was to examine the association between surgical severity, preoperative opioid use and patient characteristics with postoperative opioid prescriptions and refills.
Methods
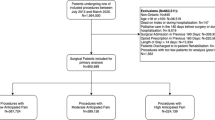
Seventy-nine patients undergoing orthopedic surgeries were reviewed. Surgical pain severity was categorized as mild (n = 25), moderate (n = 26) and severe (n = 28). Patients were also categorized as opioid naïve (n = 57), experienced (n = 16) and tolerant (n = 6). Postoperative and refill prescriptions were reviewed to determine morphine equivalent dose (MED) prescribed.
Results
Mild, moderate and severe pain surgeries received a median (interquartile range) equivalent of 20 (0, 30), 53 (33, 80) and 60 (45, 80) oxycodone 5 mg tablets, respectively. Excessive opioid prescriptions (> 400 MED) were given to 37 (46%) patients. There was no difference in the total discharge MED between moderate and severe pain surgeries or between opioid naïve and opioid-experienced patients (p > 0.05). Variables associated with excessive postoperative opioid prescriptions on multivariate analysis-included severe pain surgery (odds ratio 7.7, 95% confidence interval 2 to 25; p < 0.01) and anesthetic block (odds ratio 4.5, 95% confidence interval 1.4 to 14; p < 0.01). Variables associated with opioid refill on multivariate analysis included an American Society of Anesthiologists Physical Status (ASA) score > I (odds ratio 11, 95% confidence interval: 1.3 to 92; p < 0.01) and preoperative pain VAS (odds ratio 1.2, 95% confidence interval 1.01 to 1.4; p = 0.02).
Conclusion
The adoption of opioid prescription guidelines is warranted to differentiate between surgical severities and decrease the range and size of postoperative opioid prescriptions.
Similar content being viewed by others
References
Multiple cause of death 1999–2017 n.d. https://wonder.cdc.gov/wonder/help/mcd.html Accessed April 30 2019
Seth P, Rudd RA, Noonan RK, Haegerich TM (2018) Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health 108:500–502. https://doi.org/10.2105/AJPH.2017.304265
Seth P, Scholl L, Rudd RA, Bacon S (2018) Overdose deaths involving opioids, cocaine, and psychostimulants-United States, 2015–2016. MMWR Morb Mortal Wkly Rep 67:349–358. https://doi.org/10.15585/mmwr.mm6712a1
Morris BJ, Mir HR (2015) The opioid epidemic. J Am Acad Orthop Surg 23:267–271. https://doi.org/10.5435/JAAOS-D-14-00163
Stepan JG, Lovecchio FC, Premkumar A, Kahlenberg CA, Albert TJ, Baurley JW et al (2019) Development of an institutional opioid prescriber education program and opioid-prescribing guidelines. J Bone Jt Surg 101:5–13. https://doi.org/10.2106/JBJS.17.01645
Wyles CC, Hevesi M, Trousdale ER, Ubl DS, Gazelka HM, Habermann EB et al (2019) The 2018 Chitranjan S. Ranawat, MD Award. Clin Orthop Relat Res 477:104–113. https://doi.org/10.1007/s11999.0000000000000292
Department of orthopedic surgery adult opioid prescription guidelines n.d. https://www.mayoclinic.org/diseases-conditions/acl-injury/symptoms-causes/syc-20346173Accessed April 29 2019
ASA physical status classification system| american society of anesthesiologists (ASA) n.d. https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system Accessed January 2 2020
Hernandez NM, Parry JA, Mabry TM, Taunton MJ (2018) Patients at risk: preoperative opioid use affects opioid prescribing, refills, and outcomes after total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.01.004
Fda C. Extended-release (ER) and long-acting (LA) opioid analgesics risk evaluation and mitigation strategy (REMS). n.d
Johnson SP, Chung KC, Zhong L, Shauver MJ, Engelsbe MJ, Brummett C et al (2016) Risk of prolonged opioid use among opioid-naïve patients following common hand surgery procedures. J Hand Surg Am 41(947–957):e3. https://doi.org/10.1016/j.jhsa.2016.07.113
Stark N, Kerr S, Stevens J (2017) Prevalence and predictors of persistent post-surgical opioid use: a prospective observational cohort study. Anaesth Intensive Care 45:700–706. https://doi.org/10.1177/0310057x1704500609
Sun EC, Darnall BD, Baker LC, MacKey S (2016) Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med 176:1286–1293. https://doi.org/10.1001/jamainternmed.2016.3298
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM (2012) Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med 172:425–430. https://doi.org/10.1001/archinternmed.2011.1827
Kinjo S, Sands LP, Lim E, Paul S, Leung JM (2012) Prediction of postoperative pain using path analysis in older patients. J Anesth 26:1–8. https://doi.org/10.1007/s00540-011-1249-6
Caumo W, Schmidt AP, Schneider CN, Bergmann J, Iwamoto CW, Adamatti LC et al (2002) Preoperative predictors of moderate to intense acute postoperative pain in patients undergoing abdominal surgery. Acta Anaesthesiol Scand 46:1265–1271. https://doi.org/10.1034/j.1399-6576.2002.461015.x
Sabatino MJ, Kunkel ST, Ramkumar DB, Keeney BJ, Jevsevar DS (2018) Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg Am 100:180–188. https://doi.org/10.2106/JBJS.17.00672
Thiels CA, Ubl DS, Yost KJ, Dowdy SC, Mabry TM, Gazelka HM et al (2018) Results of a prospective, multicenter initiative aimed at developing opioid-prescribing guidelines after surgery. Ann Surg 268:457–468. https://doi.org/10.1097/SLA.0000000000002919
Gardner V, Gazzaniga D, Shepard M, Grumet R, Rubin B, Dempewolf M et al (2018) Monitoring postoperative opioid use following simple arthroscopic meniscectomy. JBJS Open Access 3:e0033. https://doi.org/10.2106/JBJS.OA.18.00033
Kim N, Matzon JL, Abboudi J, Jones C, Kirkpatrick W, Leinberry CF et al (2016) A prospective evaluation of opioid utilization after upper-extremity surgical procedures. J Bone Jt Surg 98:e89. https://doi.org/10.2106/JBJS.15.00614
Kahlenberg CA, Stepan JG, Premkumar A, Lovecchio FD, Cross MB (2019) Institutional guidelines can decrease the amount of opioids prescribed after total joint replacement. HSS J ® 15:27–30. https://doi.org/10.1007/s11420-018-9632-6
Thiels CA, Hanson KT, Cima RR, Habermann EB (2018) From data to practice. Ann Surg 267:e46–e47. https://doi.org/10.1097/SLA.0000000000002623
Hernandez NM, Parry JA, Taunton MJ (2016) Patients at risk: large opioid prescriptions after total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2017.02.060
Acknowledgements
Special thanks to Joshua King and Carrie Cherney for their assistance in data collection.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jaynstein, J., Donnell, A., Chambers, L. et al. The effect of surgical pain severity, preoperative opioid use and patient characteristics on postoperative opioid prescriptions and refills in orthopedic surgery. Eur J Orthop Surg Traumatol 30, 781–787 (2020). https://doi.org/10.1007/s00590-020-02628-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02628-z