Abstract
Background
Total hip (THA) and knee (TKA) arthroplasty are common orthopaedic procedures most frequently for older people. Whilst it is known that this older population frequently present with medical morbidities, no studies have previously documented the prevalence of such morbidities in people who have undergone THA or TKA. The purpose of this study was to determine the prevalence and what factors are in association with the presentation of medical morbidities in these populations.
Methods
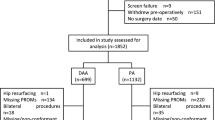
Data from the Osteoarthritis Initiative, a population-based observational study, was assessed. In total 419 people who had undergone a THA or TKA were assessed to determine the prevalence of recorded morbidities within 12 months post-arthroplasty. All medical morbidities were then assessed using univariate and then multivariate logistic regression analysis to identify factors influencing the presentation of specific morbidities at 12 months following THA or TKA.
Results
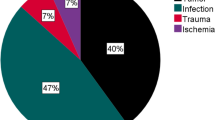
The most common medical morbidities included: osteoporosis (16 %), mild-to-moderate depression (8 %), cancer (8 %), diabetes (6 %), history of stroke or TIA (6 %) and asthma (5 %). The medical morbidities demonstrated are similar between those who undergo THA and TKA. Only gender and ethnic origin were identified as statistically significant predictors of medical morbidities in these populations. Gender was a predictor of history of heart failure, whilst ethnic origin significantly predicted depression.
Conclusions
People who undergo THA or TKA may present with a variety of medical morbidities. Accordingly consideration should be made on how to encourage the adoption and maintenance of physical activity and healthy lifestyle choices for this population.

Similar content being viewed by others
References
Arden N, Nevitt MC (2006) Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol 20:3–25
Woolf A, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ 81:646–656
NICE. Osteoarthritis—Quality standard 87. June 2015. Available at: https://www.nice.org.uk/guidance/qs87/resources/guidance-osteoarthritis-pdf. Accessed 15 May 2015
National Joint Registry. Stats online. Available at: http://www.njrcentre.org.uk/njrcentre/Healthcareproviders/Accessingthedata/StatsOnline/tabid/117/Default.aspx. Accessed on 01 Dec 2014
Reyes C, Estrada P, Nogués X, Orozco P, Cooper C, Díez-Pérez A, Formiga F, Mácias JG, Prieto-Alhambra D (2014) The impact of common co-morbidities (as measured using the Charlson index) on hip fracture risk in elderly men: a population-based cohort study. Osteoporos Int 25:1751–1758
Caughey GE, Roughead EE, Shakib S, Vitry AI, Gilbert AL (2011) Co-morbidity and potential treatment conflicts in elderly heart failure patients: a retrospective, cross-sectional study of administrative claims data. Drugs Aging 28:575–581
Tan CP, Ng A, Civil I (2004) Co-morbidities in trauma patients: common and significant. N Z Med J 117:U1044
Smith TO, Latham S, Maskrey V, Blyth A (2015) Patients’ perceptions of physical activity before and after joint replacement: a systematic review with meta-ethnographic analysis. Postgrad Med J 91(1079):483–491
Harding PA, Holland AE, Hinman RS, Delany C (2015) Physical activity perceptions and beliefs following total hip and knee arthroplasty: a qualitative study. Physiother Theory Pract 31:107–113
Radloff LS (1977) The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Hoang-Kim A, Busse JW, Groll D, Karanicolas PJ, Schemitsch E (2014) Co-morbidities in elderly patients with hip fracture: recommendations of the ISFR-IOF hip fracture outcomes working group. Arch Orthop Trauma Surg 134:189–195
de Thomasson E, Caux I, Guingand O, Terracher R, Mazel C (2009) Total hip arthroplasty for osteoarthritis in patients aged 80 years or older: influence of co-morbidities on final outcome. Orthop Traumatol Surg Res 95:249–253
Niki Y, Katsuyama E, Takeda Y, Enomoto H, Toyama Y, Suda Y (2014) Comparison of postoperative morbidity between simultaneous bilateral and staged bilateral total knee arthroplasties: serological perspective and clinical consequences. J Arthroplasty 29:504–509
Booth HP, Prevost AT, Gulliford MC (2015) Severity of obesity and management of hypertension, hypercholesterolaemia and smoking in primary care: population-based cohort study. J Hum Hypertens. doi:10.1038/jhh.2015.23
Peeler J, Christian M, Cooper J, Leiter J, MacDonald P (2015) Managing knee osteoarthritis: the effects of body weight supported physical activity on joint pain, function, and thigh muscle strength. Clin J Sport Med (in press)
Saufl N, Owens A, Kelly I, Merrill B, Freyaldenhouen LL (2007) A multidisciplinary approach to total joint replacement. J Perianesth Nurs 22:195–206
Heidari B, Hosseini R, Javadian Y, Bijani A, Sateri MH, Nouroddini HG (2015) Factors affecting bone mineral density in postmenopausal women. Arch Osteoporos 10:217
Black SV, Cooper R, Martin KR, Brage S, Kuh D, Stafford M (2015) Physical activity and mental well-being in a cohort aged 60–64 years. Am J Prev Med 49(2):172–180
Hamasaki H, Noda M, Moriyama S, Yoshikawa R, Katsuyama H, Sako A, Mishima S, Kakei M, Ezaki O, Yanai H (2015) Daily physical activity assessed by a triaxial accelerometer is beneficially associated with waist circumference, serum triglycerides, and insulin resistance in Japanese patients with prediabetes or untreated early type 2 diabetes. J Diabetes Res 2015:526201
Ma J, Strub P, Xiao L, Lavori PW, Camargo CA Jr, Wilson SR, Gardner CD, Buist AS, Haskell WL, Lv N (2015) Behavioral weight loss and physical activity intervention in obese adults with asthma. A randomized trial. Ann Am Thorac Soc 12:1–11
Spring B, Moller AC, Colangelo LA, Siddique J, Roehrig M, Daviglus ML, Polak JF, Reis JP, Sidney S, Liu K (2014) Healthy lifestyle change and subclinical atherosclerosis in young adults: Coronary Artery Risk Development in Young Adults (CARDIA) study. Circulation 130:10–17
Acknowledgments
We would like to thank Professor Andy Jones, Professor in Public Health, Norwich Medical School, the University of East Anglia, for reviewing this paper during its preparation.
Funding
The OAI is a public–private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethics approval
Committee on Human Research, University of California, San Francisco (IRB Approval Number 10-00532 Approved 10th March 2015).
Data sharing statement
This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Smith, T.O., Penny, F. & Fleetcroft, R. Medical morbidities in people following hip and knee arthroplasty: data from the Osteoarthritis Initiative. Eur J Orthop Surg Traumatol 26, 99–106 (2016). https://doi.org/10.1007/s00590-015-1713-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-015-1713-3